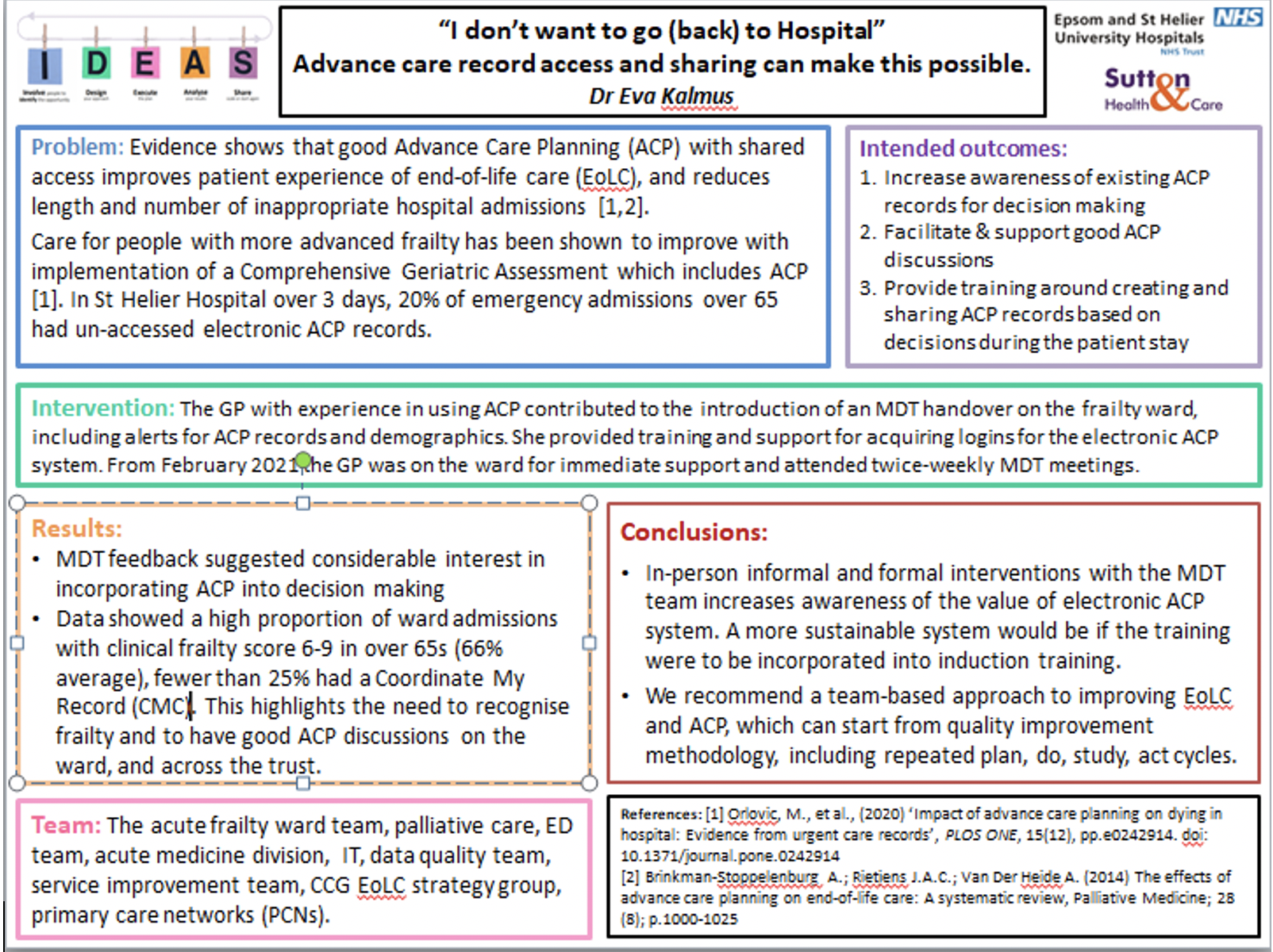
Dr Eva Kalmus, an Interface Medicine GP at Epsom and St Helier University Hospitals NHS Trust led a Quality Improvement Project with teams across the Trust (acute frailty ward team, palliative care, ED team, acute medicine division, IT, data quality team, and service improvement team) as well as the CCG end-of-life care (EoLC) strategy group and primary care networks (PCNs).
Background
Evidence shows that good Advance Care Planning (ACP) with shared access improves patient experience of EoLC, and reduces length and number of inappropriate hospital admissions [1,2]. Care for people with more advanced frailty has been shown to improve with implementation of a Comprehensive Geriatric Assessment which includes ACP [1]. In St Helier Hospital over 3 days, 20% of emergency admissions over 65 had un-accessed electronic ACP records.
Intervention
The GP with experience in using ACP contributed to the introduction of an MDT handover on the frailty ward, including alerts for ACP records and demographics. The GP provided training and support for acquiring logins for the electronic ACP system. From February 2021 the GP was on the ward for immediate support and attended twice-weekly MDT meetings.
Intended outcomes
• Increase awareness of existing ACP records for decision making
• Facilitate & support good ACP discussions
• Provide training around creating and sharing ACP records based on decisions during the patient stay
Results
MDT feedback suggested considerable interest in incorporating ACP into decision making.
Data showed a high proportion of ward admissions had a clinical frailty score 6-9 among the over 65s (66% average) for whom hospital admission and some interventions carry significant risks of harm. Under 25% had an electronic ACP record. This highlights the need to recognise frailty and to have good ACP discussions on the ward, and across the Trust.
Conclusions
In-person informal and formal interventions with the MDT team increases awareness of the value of electronic ACP system. A more sustainable system would be if the training were to be incorporated into induction training.
We recommend a team-based approach to improving EoLC and ACP, which can start from quality improvement methodology, including repeated plan, do, study and act cycles.
References: [1] Orlovic, M., et al., (2020) ‘Impact of advance care planning on dying in hospital: Evidence from urgent care records’, PLOS ONE, 15(12), pp.e0242914.
[2] Brinkman-Stoppelenburg A.,Rietjens J.A.C.,Van Der Heide A. (2014) ‘The effects of advance care planning on end-of-life care: A systematic review’, Palliative Medicine; 28 (8); p.1000-1025.
You can read and download the full project poster HERE