Streamlining the Newborn Infant Physical Examination (NIPE) Process on the Maternity Ward to Improve Productivity.
Quality Improvement Presenter(s):
Katy Murphy (Advanced Neonatal Nurse Practitioner)
Sarah Simmons (Advanced Neonatal Nurse Practitioner)
Background & Problem:
This project aims to improve the NIPE process for infants on the Maternity Ward at Gloucester Royal Hospital. All infants receive a NIPE within 72 hours of birth, typically before discharge.
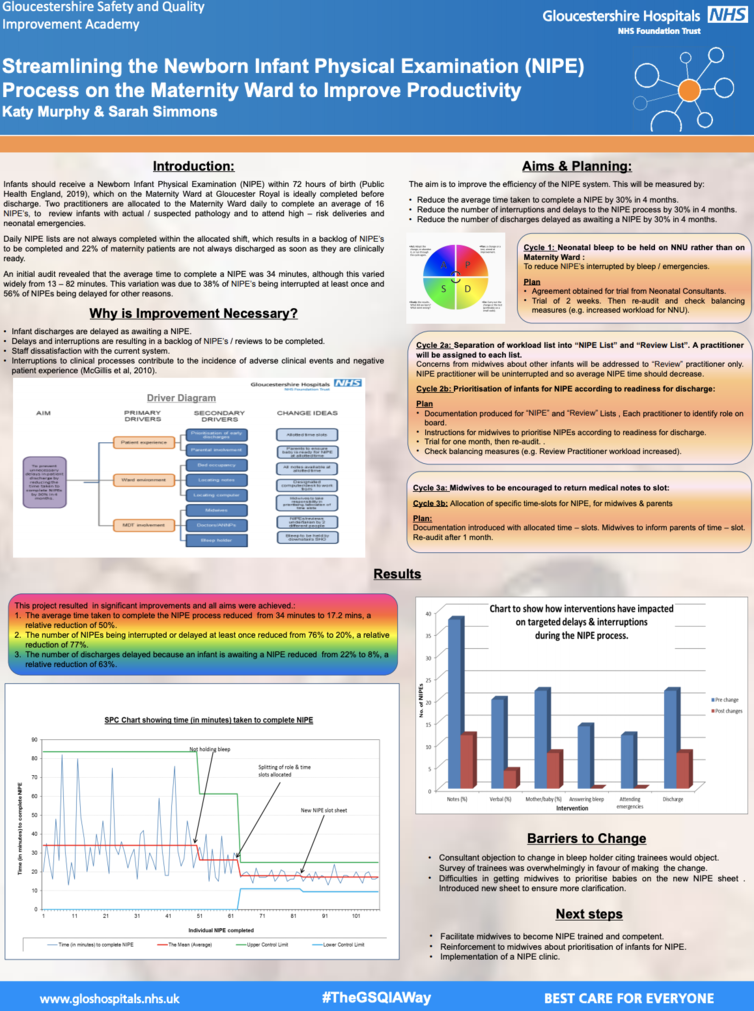
Due to workload, there is often a backlog NIPE’s, with 22% of infants consequently having discharge delayed. An audit identified the time to complete a NIPE varied from 13 – 82 minutes, with an average time of 34 minutes. Variation was attributed to interruptions and delays with 38% of NIPE’s interrupted at least once e.g. to respond to bleep (14%), attend a delivery / emergency (12%) or respond to midwifery concerns (28%). Also 56% of NIPE’s suffered at least one delay for other reasons, including misplaced notes (38%) and unavailability of mother or baby (22%).
We aimed to improve the process by reducing interruptions and delays, which would ultimately reduce the average time taken to complete the NIPE and reduce discharge delays.
SMART Aims:
1) Reduce average time taken to complete a NIPE by 30% in 4 months.
2) Reduce percentage of interruptions and delays to the NIPE process by 30% in 4 months.
3) Reduce percentage of discharges delayed as awaiting a NIPE by 30% in 4 months.
Method:
• Engagement of key stakeholders.
• Baseline audit detailing time taken to complete NIPE and delays or interruptions.
• Neonatal bleep to be help on NNU rather than Maternity Ward.
• Separation of NIPE and Review workload and timed slots.
• Prioritisation of infants according to readiness for discharge.
• Medical notes to be returned to slot.
Results:
All project aims were achieved.
1) The average time taken to complete the NIPE process reduced from 34 minutes to 17.2 minutes, a relative reduction of 50%.
2) The number of NIPE’s being interrupted or delayed at least once reduced from 76% to 20%, a relative reduction of 77%.
3) The number of discharges delayed because infant is awaiting a NIPE reduced from 22% to 8%, a relative reduction of 63%
Lessons Learnt:
Making process changes works best when all stakeholders are aware of the rationale.
Be prepared to provide evidence for the changes you want to make to key stakeholders.
Next steps:
To facilitate more midwives to be able to do NIPEs by providing assessment to those in training and participating in refresher conferences.
Potentially take improvements further by initiating a NIPE and neonatal in-reach clinic.