Background & Problem
Liver disease is the only major cause of death still increasing year-on-year, twice as many people now die from liver disease as in 1991. From the Bereavement Voices Survey it was found where Liver disease was mentioned , carers were more likely to rate the coordination of care as not working well together compared to other illnesses.
People dying from Liver disease often have complex end of life care needs and >70% die in hospital, even though this is not necessarily their wish. From our experience, patients are unaware of their poor prognosis and therefore have not had any discussions regarding their wishes in end of life. This means that when a patient deteriorates suddenly, it can be too late to have these discussions, therefore their wishes not known and also patient and family are often unprepared.
Aim
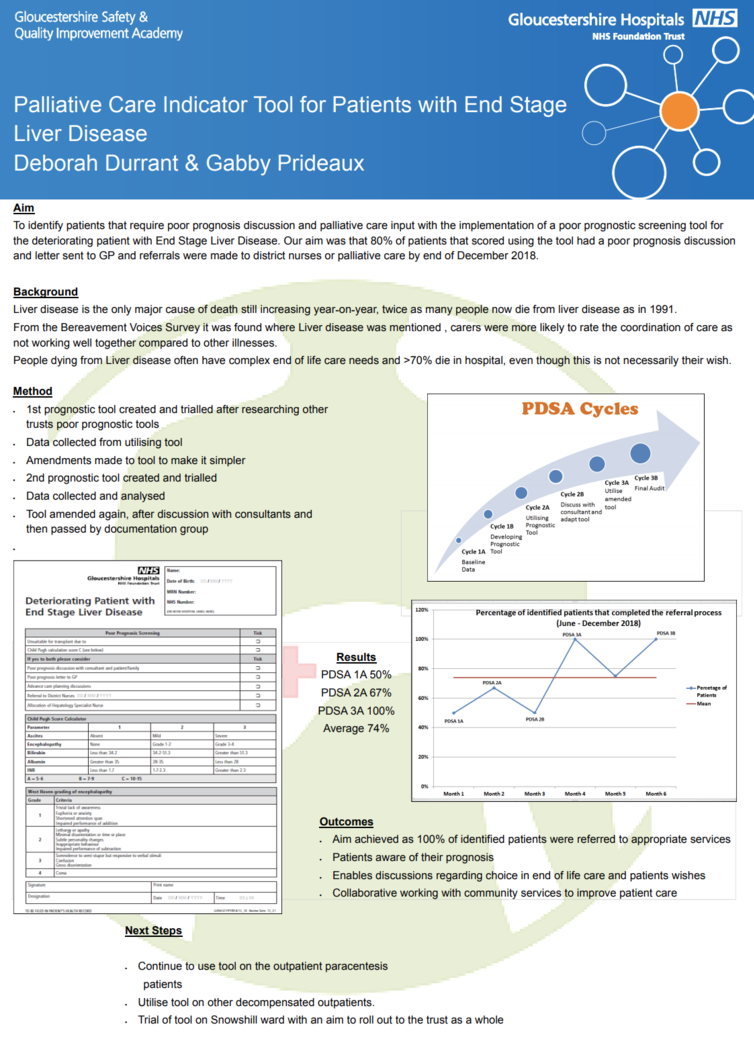
To identify patients that require poor prognosis discussion and palliative care input with the implementation of a poor prognostic screening tool for the deteriorating patient with End Stage Liver Disease. Our aim was that 80% of patients that scored using the tool had a poor prognosis discussion and letter sent to GP and referrals were made to district nurses or palliative care.
Method
After researching poor prognosis tools used by other trusts and discussing ideas with the lead hepatology consultant, we created our own Palliative Care Indicator tool. Using the tool, we assessed appropriate patients that had decompensated liver disease who attended the Medical Day Unit for paracentesis.
Results
Looking at the baseline date the number of patients who had poor prognosis discussion, referral to district nurses or palliative care and poor prognosis letter to GP was 50%. After 6 months of using the tool this had improved to 100%.
This meant that patients were more aware of their prognosis, which enabled an open discussion, therefore allowing more choice in regards to end of life care, for example chosen place of death. It also meant that patients were better supported in the community as district nurses or palliative care are aware of their needs and can carry out their own assessments. This in turn has encouraged working alongside the community teams which has allowed us to work collaboratively to achieve the best care for patients.
Implications
It has highlighted the importance of patients being assessed as soon as it’s appropriate to allow these discussions to be had, as it had become apparent that previously patients were unaware of their poor prognosis, which meant sometimes their wishes were not discussed in time.
Now that the tool has been passed by the documentation group, we intend to roll this out to the gastroenterology ward in CGH, with the overall aim for it to be utilised by the trust as a whole.
Quality Improvement Presenter(s)
Deborah Durrant - Senior Liver Specialist Nurse
Gabby Prideaux - Liver Specialist Nurse
Quality Improvement Team
Dr Coral Hollywood – Lead Hepatology consultant
