Background & Problem
Chemotherapy induced hair loss is a common side effect of cancer treatment that can have a traumatic and distressing impact on some patients. Scalp cooling can prevent chemotherapy induced hair loss in some patients receiving certain chemotherapy regimens.
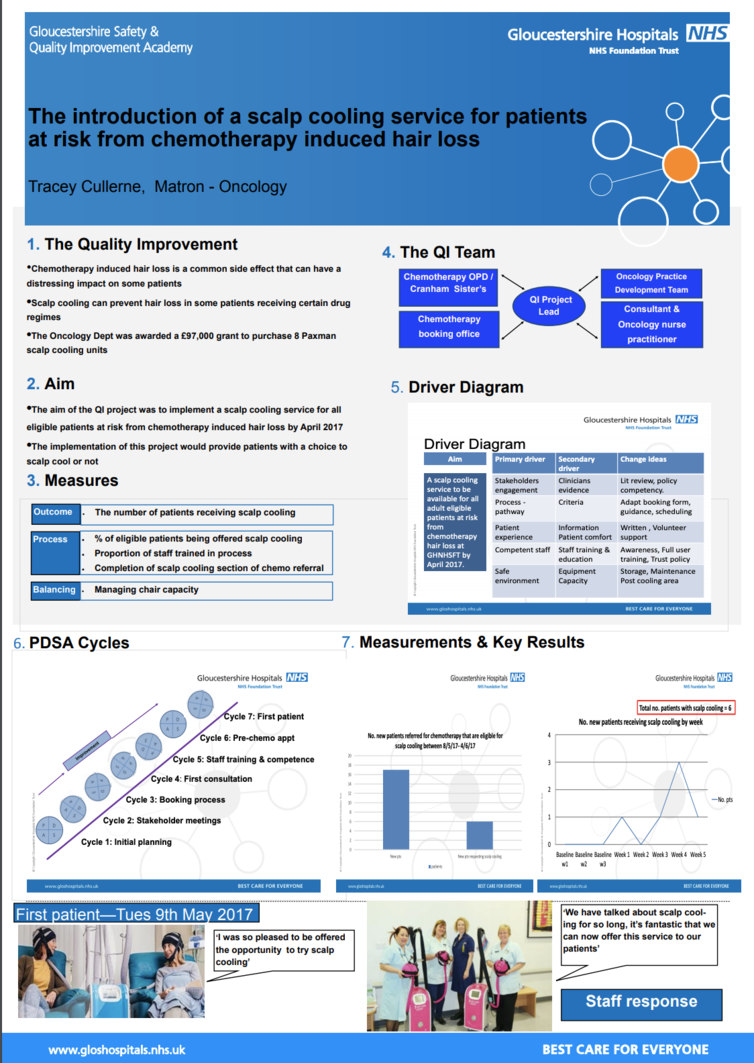
In Sept 2016 the Oncology Dept was awarded a £97,000 grant to purchase 8 Paxman scalp cooling units to implement a scalp cooling service. A working group was established to develop a patient pathway to introduce this service for our patients.
Aim
The aim of the project was to implement a scalp cooling service for all eligible patients at risk from chemotherapy induced hair loss by April 2017.
Method
A comprehensive literature review was undertaken and evidence presented to Chemotherapy sub-group to gain a position statement and support. A working group was then established to develop a patient pathway, booking criteria & guidelines, patient information, Trust policy & action cards, co-ordinate staff awareness sessions, provide full user training and develop a staff training competency. Meetings were held 2 weekly between Feb -May 17 to monitor progress, agree actions and plan next steps.
Results
A scalp cooling service has successfully been implemented within the Oncology dept. It has provided patients with the opportunity to regain some control during their chemotherapy treatment as they have a choice to try scalp cooling. The service is currently available for patients receiving chemotherapy for breast cancer. Our first patient was treated on Mon 8th May 2017; she stated ‘I was so pleased to be given the opportunity to try scalp cooling’.
Implications
The working group will continue to meet so that we can plan to extend the service to all eligible patients at risk from chemotherapy induced hair loss so they have the choice to try scalp cooling or not. A patient and staff questionnaire is to be developed so feedback can be obtained, learning can be shared and practice improved.
From my experience it absolutely vital your Quality Improvement team consists of people that are going to be involved in the entire patients journey…they will understand their ‘part of the journey’ and be able to fully inform the QI team, influence their colleagues and provide support. As QI lead for the project my role has been to listen, communicate, support and set achievable goals (deadlines!!). It has been a rewarding project as I know this service is directly improving patient care and choice.
Quality Improvement Presenter(s)
Tracey Cullerne, Matron, Oncology
Quality Improvement Team
Alison Peett, Oncology Practice Develop Facilitator
Julie Ford, Senior Sister Chemotherapy OPD
Sally Burge, Senior Sister Cranham Suite
Dr Jo Bowen, Consultant Oncologist
Chris Sullivan, Oncology Administration Manager
Val Fielding, Health Care Assistant Chemotherapy OPD
Di Townsend, Health Care Assistant Cranham Suite
Louise Kidner, Oncology Nurse Practitioner
Dr Colin Binks, Specialty Associate Oncology Doctor
Dr Charlie Candish, Quality Improvement Project Sponsor
