Background & Problem
Patients presenting to the Emergency Department with a headache must have potentially life-threatening causes, such as raised intracranial pressure, excluded. Funduscopic examination (looking at the retina with an ophthalmoscope or a retinal camera) can reveal papilloedema (swollen optic discs on the retina) indicating raised intracranial pressure. However, there are many barriers to performing fundoscopy.
Aim
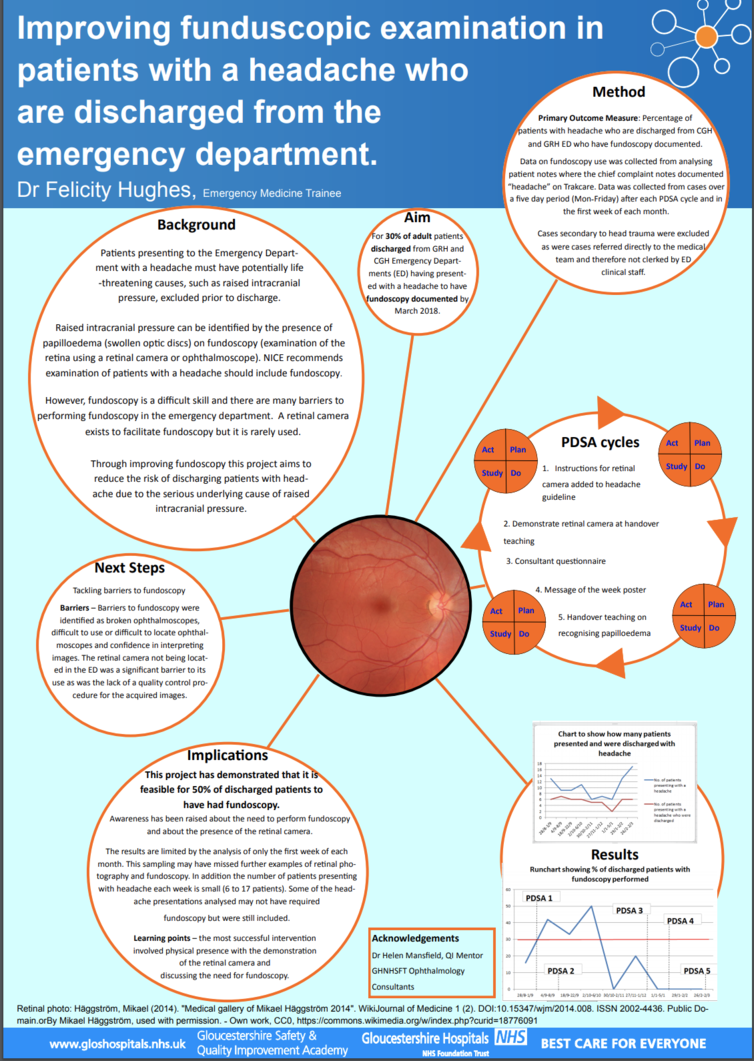
For 30% of adult patients discharged from GRH and CGH Emergency Departments having presented with a headache to have fundoscopy documented by March 2018.
Method
PDSA 1 – Instructions for retinal camera added to headache guideline
PDSA 2 – Demonstrate retinal camera at handover teaching
PDSA 3 – Consultant questionnaire
PDSA 4 – Message of the week poster
PDSA 5 – Handover teaching on recognising papilloedema
Primary Outcome Measure: Percentage of patients with headache who are discharged from CGH and GRH Emergency Department who have fundoscopy documented.
Data was collected from analysing patient notes where the chief presenting complaint documented “headache” on Trakcare. Cases secondary to head trauma were excluded as were cases referred directly to the medical team. Data was collected over a five day period (Mon-Friday) after PDSA cycles and in the first week of each month.
Results
In the first three months which followed PDSAs 1 and 2 there was an improvement in the percentage of patients having fundoscopy performed. However this improvement was not maintained. The retinal camera was only used twice over the 6 months.
Implications
This project has demonstrated that it is feasible for 50% of discharged patients to have had fundoscopy performed. Awareness has been raised about the need to perform fundoscopy and about the presence of the retinal camera.
Learning points – the most successful intervention involved physical presence in the Emergency Department with the demonstration of the retinal camera and discussing the need for fundoscopy.
Next Steps:
Tackling the barriers to fundoscopy
- broken ophthalmoscopes, difficult to use or difficult to locate ophthalmoscopes and confidence in interpreting images
- Retinal camera not located in ED
- Lack of quality control of retinal camera images.
Quality Improvement Presenter
Dr Felicity Hughes, CT2 Emergency Medicine trainee
Quality Improvement Team
Dr Helen Mansfield, Emergency Medicine Consultant, QI mentor