Context and relevance to patient safety
Hospital falls and subsequent harm with increased morbidity are a common and preventable event in secondary care. Cost of falls has been calculated to be in the region of £634 million a year.
Problem
Lack of knowledge and understanding regarding prevention of falls by the multi-disciplinary team which in turn led to poor compliance with implementation and documentation of falls care plan and subsequent patient falls.
Aim
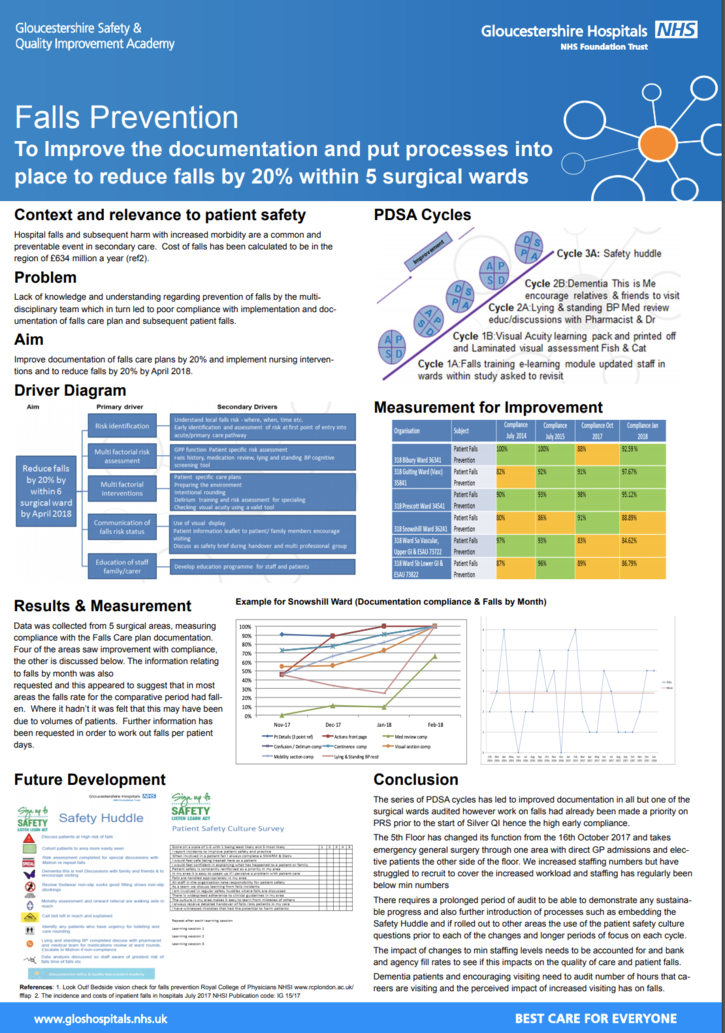
Improve documentation of falls care plans by 20% and implement nursing interventions and to reduce falls by 20% by April 2018.
Method
Data was collected from 5 surgical areas, measuring compliance with the Falls Care plan documentation. Four of the areas saw improvement with compliance, the other is discussed below. The information relating to falls by month was also requested and this appeared to suggest that in most areas the falls rate for the comparative period had fallen. Where it hadn’t it was felt that this may have been due to volumes of patients. Further information has been requested in order to work out falls per patient days.
Results
In the first three months which followed PDSAs 1 and 2 there was an improvement in the percentage of patients having fundoscopy performed. However this improvement was not maintained. The retinal camera was only used twice over the 6 months.
Implications
The series of PDSA cycles has led to improved documentation in all but one of the surgical wards audited however work on falls had already been made a priority on PRS prior to the start of Silver QI hence the high early compliance.
The 5th Floor has changed its function from the 16th October 2017 and takes emergency general surgery through one area with direct GP admissions and elective patients the other side of the floor. We increased staffing numbers but have struggled to recruit to cover the increased workload and staffing has regularly been below min numbers
There requires a prolonged period of audit to be able to demonstrate any sustainable progress and also further introduction of processes such as embedding the Safety Huddle and if rolled out to other areas the use of the patient safety culture questions prior to each of the changes and longer periods of focus on each cycle.
The impact of changes to min staffing levels needs to be accounted for and bank and agency fill rates to see if this impacts on the quality of care and patient falls.
Dementia patients and encouraging visiting need to audit number of hours that careers are visiting and the perceived impact of increased visiting has on falls.
Quality Improvement Presenter(s)
Rob Randles
Quality Improvement Team
Nicola Holton divisional risk manager
Philip Lort Practice Development & Educational Support Nurse (Surgical Division)
Carys Hoskins Lead Surgical Pharmacist CGH
Sr Russell & team 5th Floor
Sr Beasley & team Bibury ward
Sr Harvey & team Snowshill ward
Sr Jones & team Guiting ward
Sr Harker & team Prescott ward
