Simulation is a method to provide an experiential learning environment whereby learners can acquire, refine and maintain skills without impacting on patient safety (Hussein et al, 2021, McKimm et al, 2017). Simulation based activities within the classroom setting can be similar to the “real world”; therefore, it is accepted that knowledge and skills acquired can be transferable to real situations (Joyce et al, 2008).
Lane et al (2001) identified that simulation within medical education is an integral part of the curricula, both in undergraduate and postgraduate programmes. Despite the length of time since this review, simulation continues to be a regular teaching strategy for medical students, junior doctors and other health care professions (McKimm et al, 2017). Learners can acquire essential skills during simulation which they may have limited exposure to in the clinical setting. The General Medical Council [GMC] (2018) mandate a list of leadership and teamworking outcomes for graduates; simulation can expose learners to situations whereby they can apply these non-technical skills in a psychologically “safe space” (Watts et al, 2021).
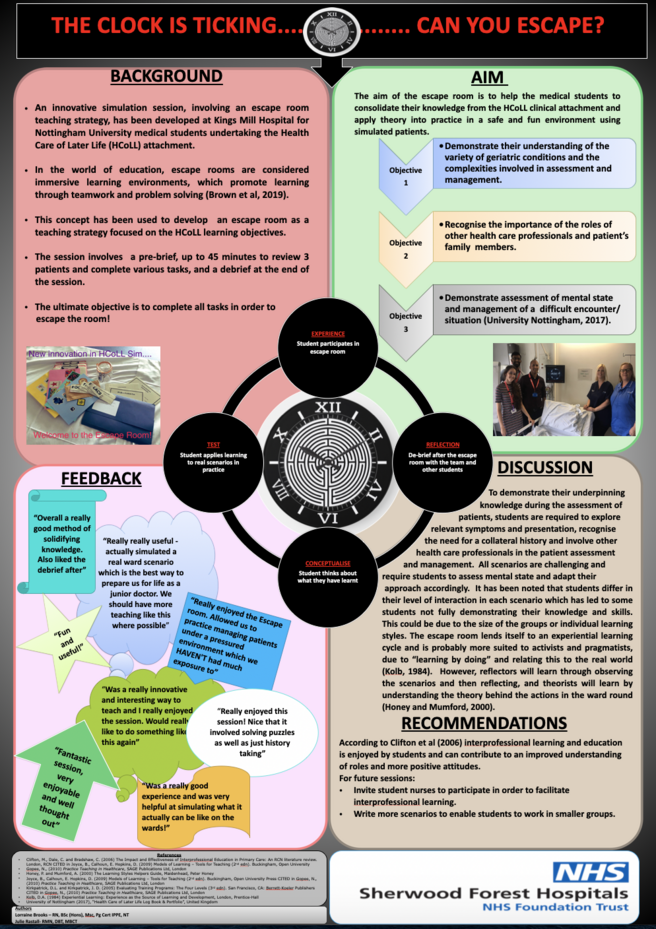
A simulation session involving an escape room teaching strategy has been designed for fourth year medical students undertaking the Health Care of Later Life attachment at the local Trust. Locally, feedback from medical students on simulation sessions has been overwhelmingly positive with students wanting more and more sessions.
In the world of education, gamification, which uses games in non-game settings, has been shown to motivate learners and increase engagement within the learning environment (Guckian et al, 2020). Escape rooms are considered immersive learning environments, which promote learning through teamwork and problem solving (Brown et al, 2019). Escape room simulations require learners to accomplish a series of tasks, drawing on multiple skills that are critical in the delivery of patient care, such as communication, teamwork, critical thinking, and leadership (Larcom, 2021).
The theme of the simulation involves geriatric medicine cases using simulated patients. The learning outcomes are based on the curriculum from the medical school in relation to knowledge requirements, as well as, communication, team working, prioritisation and leadership. There are three to four students participating in the simulation; the students are exposed to situations that they will be expected to manage as a junior doctor. In a study by Boostel et al (2018) the realism and demands during a simulation helps to prepare pre-registration students for the realities of practice. The time pressures and unexpected events within the escape room mimic the pressure of the workload of a junior doctor on a geriatric ward. Therefore, the design of the simulation, using authentic patient scenarios and creating the feeling of working on a busy ward environment, can help the medical students prepare for life as a junior doctor.
The session structure involves a pre-brief, then up to 45 minutes to review 3 patients (in the simulation ward) involving various tasks and puzzles; the aim being to complete all tasks and puzzles within the time allotted to escape the room. This is followed by a debrief at the end of the session. The students are advised to work as a team, prioritise accordingly and react to the changing situation within the simulation.
Click on the image below to read and download the poster