Introduction
As NHS staff, we strive to provide the most efficient and high-quality care possible for our patients. The discharge process is key to this, aiming to get patients home as soon as is safe and appropriate for them, and opening up beds for those who need them next. Criteria-led discharge (CLD) is an effective solution which reduces length of stay and empowers staff and patients.
What is Criteria-Led Discharge?
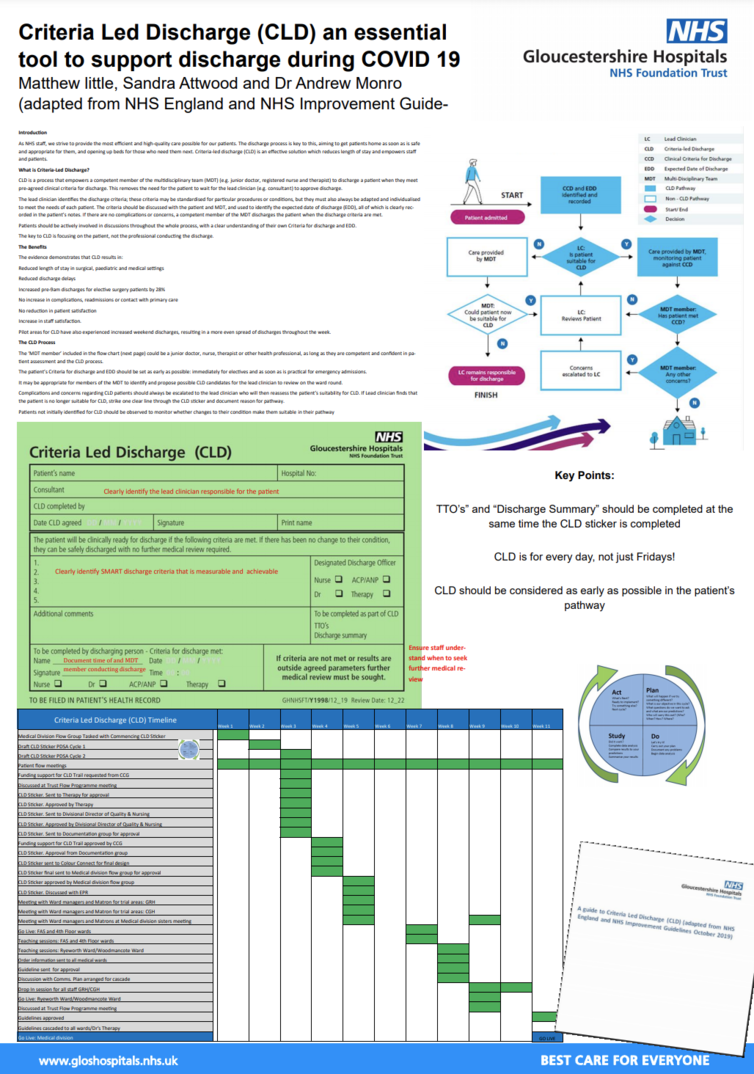
CLD is a process that empowers a competent member of the multidisciplinary team (MDT) (e.g. junior doctor, registered nurse and therapist) to discharge a patient when they meet pre-agreed clinical criteria for discharge. This removes the need for the patient to wait for the lead clinician (e.g. consultant) to approve discharge.
The lead clinician identifies the discharge criteria; these criteria may be standardised for particular procedures or conditions, but they must also always be adapted and individualised to meet the needs of each patient. The criteria should be discussed with the patient and MDT, and used to identify the expected date of discharge (EDD), all of which is clearly recorded in the patient’s notes. If there are no complications or concerns, a competent member of the MDT discharges the patient when the discharge criteria are met.
Patients should be actively involved in discussions throughout the whole process, with a clear understanding of their own Criteria for discharge and EDD.
The key to CLD is focusing on the patient, not the professional conducting the discharge.
The Benefits
The evidence demonstrates that CLD results in:
Reduced length of stay in surgical, paediatric and medical settings
Reduced discharge delays
Increased pre-9am discharges for elective surgery patients by 28%
No increase in complications, readmissions or contact with primary care
No reduction in patient satisfaction
Increase in staff satisfaction.
Pilot areas for CLD have also experienced increased weekend discharges, resulting in a more even spread of discharges throughout the week.
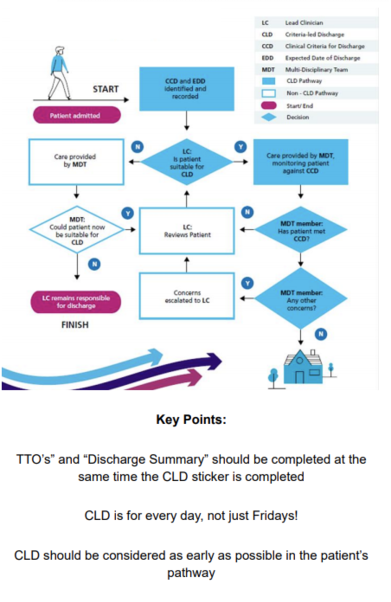
The CLD Process
The ‘MDT member’ included in the flow chart (next page) could be a junior doctor, nurse, therapist or other health professional, as long as they are competent and confident in patient assessment and the CLD process.
The patient’s Criteria for discharge and EDD should be set as early as possible: immediately for electives and as soon as is practical for emergency admissions.
It may be appropriate for members of the MDT to identify and propose possible CLD candidates for the lead clinician to review on the ward round.
Complications and concerns regarding CLD patients should always be escalated to the lead clinician who will then reassess the patient’s suitability for CLD. If Lead clinician finds that the patient is no longer suitable for CLD, strike one clear line through the CLD sticker and document reason for pathway.
Patients not initially identified for CLD should be observed to monitor whether changes to their condition make them suitable in their pathway
The lead clinician always retains responsibility for patients. This responsibility does not transfer to the MDT member conducting the patients’ discharge. There must be a clear process for escalating concerns and handing back to the lead clinician.
You can find the full project outcomes HERE
