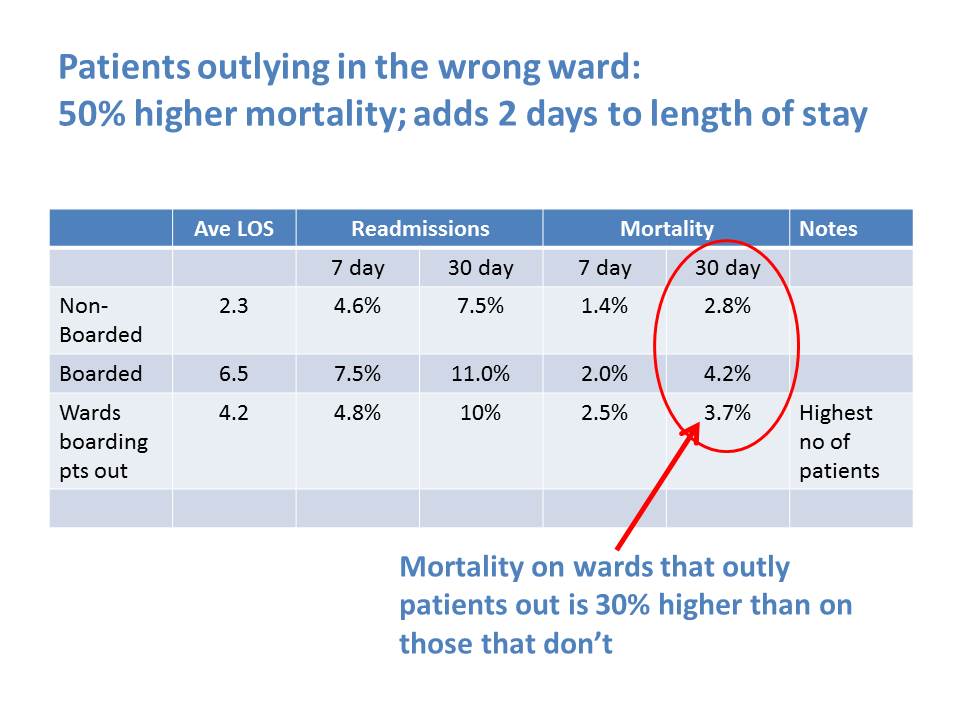
Outliers were a chronic problem for many years in our organisation and indeed in many organisations I have visited. About 2 years ago a colleague shared research project undertaken in Scotland that highlighted the actual harm caused to patients. This, coupled with the operational difficulties of managing outliers was a key driver to deliver a step change in managing flow and placing patients.
The bed managers were taking the lead in placing patients in beds and although clinical they did not have the specific clinical expertise that separates a true respiratory patient from a patient with an associated general medical problem but not requiring specialist input. We needed to find a way of wards recognising their demand but also managing it. We introduced patient mapping where the ward manager in liaison with the consultant goes to the assessment units and ED at regular slots throughout the day and selects their patients. Therefore admissions are being led by the ward and not by the bed manager.
There needs to be a piece of cheese/ an incentive to embed the behaviour. It's simple but effective when ward managers realise that they are in control of who comes to their ward, it reduces LOS and for the consultants it removes outliers. The process needs to be micromanaged to start with and led by someone senior to get traction. There needs to be rigor in the attendance from the wards at fixed times throughout the day and a record of attendance. Each ward needs to chose patients for their specialties but also there needs to be a fair share of general medicine. We ask that every ward selects 2 specialty patients and 2 general. If there are 4 specialty pts then that's the 4 they get to take.
I found that when ward staff introduced themselves to the patients that they were planning to admit, the relationship commenced and created another incentive to ensure they got them on their ward. A great example was in respiratory were the wards had approx 50-60% respiratory and the rest were general medicine or other specialist medicine yet there were still respiratory outliers. The 2 ward managers proactively visited the assessment units and ED at regular slots throughout the day and not only mapped the patient to their wards but proactively pulled them through. This was because they could see the impact of having their wards full with respiratory patients and the outcomes for patients.
Each ward knows what their average demand is per day and therefore they plan to take 40% by lunchtime. These are usually patients from the previous night who were mapped at 6pm, the names are on the ward boards (like a TCI) list and the nurse in charge is responsible for pulling them through from the assessment areas. There are still some challenges when the discharge picture is weak but generally we have reduced outliers by 90% and this has been mostly sustained for the past 10 months.
Mairead Mc Cormick - Deputy COO, Barking, Havering and Redbridge NHS Trust
