Patient flow has become an all year round issue for health and social care systems to endure, no longer is patient flow pressures just a winter months agony. The reality today is ‘winter pressures’ are discerned through the summer months too.
The practical principles of patient flow must be endorsed as ‘business as usual’ in the operational setting. Delivering good practice of timely hospital discharges every day of the year is achievable when services are ‘integrated’. Efficiency at every step of a patient/client caring need including discharge particularly when integration of systems, inclusive of personnel and practices, are evident between health and social care
Amalgamating the principles of patient flow into established clinical wards is possible to accomplish operational success on a daily basis. This then goes some way to enable the system, coping with patient flow pressures, to acquire efficient flow at the hospitals front door being Emergency Department. The process to establish patient flow into the wards is achievable when a dedicated systematic approach of support, rapport and focus endorsing simple patient flow practices become ‘business as usual’.
The challenge being to improve patient flow and success is measured from the resulting DTOC reduction with the consequence of empty bed availability to transfer patients into.
The success of the in-patient flow plan was measured over a twelve week period in 2018, resulted in:
• A reduction of DTOC by 8% over a 3 month period
• The reality demonstrated 107 extra bed days over this period
• Reflected on a daily basis with a peak of up to 20 available beds to admit into.
The approach to deliver a plan of improving the throughput of timely admissions and discharge into the clinical ward areas was to initially build a rapport underpinned by trust and mutual respect. Then to undertake a period of diagnostics using the framework of a ‘Discharge Bundle’, as previously described in FabStuff 02/12/16, to inform the priority of action.
The key elements of actions were diagnosed as:
• Tighten the focus on patient flow principles
• Fine tune daily patient flow practices
• Health professionals encouraged to value their relationship with social care professionals to enable a much greater involvement with two way dialogue
• Establish formal integrated DTOC processes between health and social care systems
• Engaged in a healthy daily dialogue between health and social care professionals at a senior operational level to actively resolve and predict blocks in patients discharge plans
• Implemented a process of ‘escalation’, being the key element to continued patient flow victory!
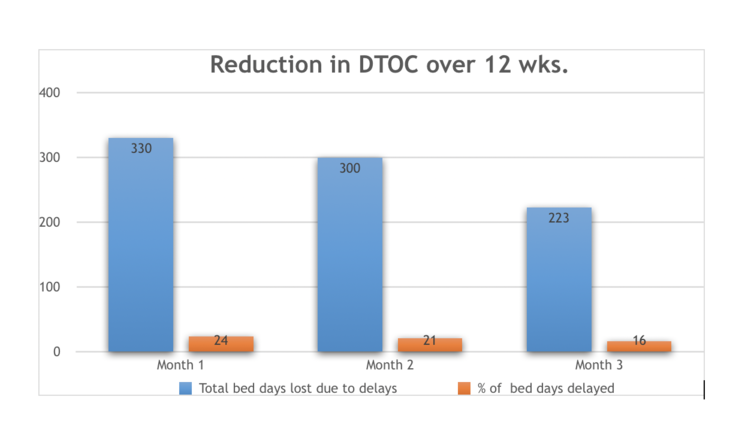
Some 5 months, in total, having followed the transformation in patient flow plans the division denote a continued DTOC’s reduction to just 9% of the total divisional bed base with a further planned trajectory to achieve more DTOC reductions
Improving patient flow in the hospital ward setting goes some way to impact on the overall picture of system wide pressure to support patients discharged to their own homes safely in the best possible health.