Introduction
The SAFER patient flow bundle is a practical tool to reduce delays for patients in adult inpatient wards (excluding maternity).When followed consistently, length of stay reduces and patient flow and safety improves.
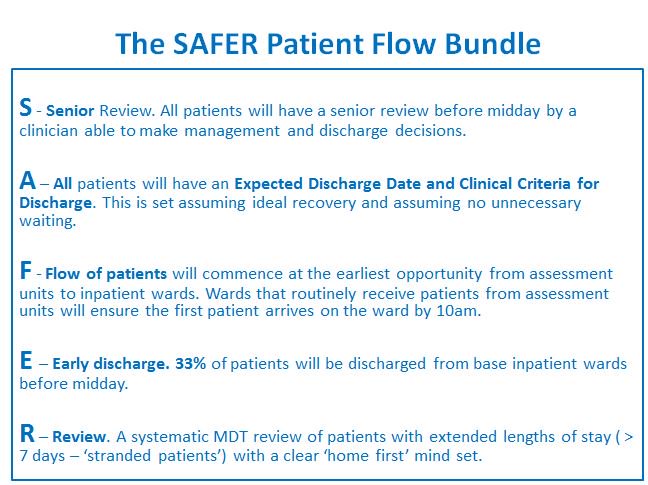
The SAFER bundle blends five elements of best practice. It’s important to implement all five elements together to achieve cumulative benefits. The SAFER patient flow bundle works particularly well when it is used in conjunction with the ‘red & green days’ approach.
The SAFER patient flow bundle
S - Senior Review. All patients will have a senior review before midday by a clinician able to make management and discharge decisions.
A – All patients will have an Expected Discharge Date and Clinical Criteria for Discharge. This is set assuming ideal recovery and assuming no unnecessary waiting.
F - Flow of patients will commence at the earliest opportunity from assessment units to inpatient wards. Wards that routinely receive patients from assessment units will ensure the first patient arrives on the ward by 10am.
E – Early discharge. 33% of patients will be discharged from base inpatient wards before midday.
R – Review. A systematic MDT review of patients with extended lengths of stay ( > 7 days – ‘stranded patients’) with a clear ‘home first’ mind set.
S - Senior Review. All patients should have a senior review before midday
It’s important to use simple rules to standardise ward and board round processes. Minimising unwarranted variation between individual clinicians and clinical teams ensures that all patients receive an effective daily senior review.
Daily review by a senior clinician able to make management and discharge decisions is essential seven days a week. Effective ward and board rounds are crucial to decision making and care co-ordination.
Ward rounds. Ward rounds should add value and lead to clear actions that are written in the notes and acted upon. For a detailed description of ward round best practice see the joint RCP/RCN guidance.
Effective ward rounds:
- Use check lists to reduce variation and prevent actions being omitted.
- Always include a qualified nurse, other members of the multidisciplinary team and involve the patient.
- Are led by a ‘consultant of many days’, who focuses on the management of ward patients while her specialty colleagues focus on elective and other activities.
- Are ‘one-stop’ ward rounds, where most tasks (e.g. the writing up of TTOs or the ordering of a scan) are completed before the round moves onto the next patient? This avoids overloading junior staff, batching tasks and creating delays.
- Use a computer on wheels as an enabler.
Red and Green Days. This is a useful approach to optimising flow. The team on the round discusses whether the patient’s day ahead is ‘red’ (a day where there is little or no value adding care) or ‘green’ (a day of value for the patient’s progress towards discharge). This is repeated for every patient. If the day ahead is likely to be a ‘red’ day, action needs to be agreed by the team to create a ‘green’ day for the patient.
The purpose of board rounds is to ensure that patients’ case management plans are progressed so that as many days as possible become ‘green days’. If patients require an investigation to progress their care, then the day will only become green if investigations occur that day and there is a clear plan of what the action with regard to the results will be. Where patients have not met their ‘clinical criteria for discharge’ and are receiving active interventions to get them to that state by tomorrow, the day is only a ‘green bed day’ if the discharge prescription medications (TTOs/TTAs) are ready by the evening before the expected date of discharge. The causes of red days should be recorded so that common causes of delays can be identified and addressed.
Measuring compliance with the ‘S'of SAFER - senior review - is important. During early afternoon bed meetings, the number of patients who have not had a senior review should be highlighted, discussed and mitigating actions taken. On going measurement of day to day compliance using SPC run charts (statistical process control) should be measured so it is really clear how many patients are receiving a senior review before midday every day and trends.
A - All patients will have an expected discharge date (EDD) and clinical criteria for discharge (CCD)
All patients should have a consultant approved care plan containing an EDD and CDD, set within 14 hours of admission.
Clinical criteria for discharge should include physiological and functional criteria, but should not be about medically ‘optimising’ a patient or returning them to their pre-admission baseline. A period of post-hospital recovery and rehabilitation should be anticipated and allowed for.
EDDs should be set by a consultant with the multi-disciplinary team. EDDs represent a professional judgement of when a patient is anticipated to achieve his/her clinical and functional goals (CCDs) and can leave hospital to recover or rehabilitate in a non-acute setting (usually in their normal place of residence).
It is more important that a challenging EDD ‘goal’ is set and worked to by the team than getting the EDD exactly ‘right’. Clear goals reduce procrastination and help galvanise teams to work together to focus on getting patients home promptly.
The progress of every patient towards his/her EDD should be assessed every day at a board or ward round led by a senior clinical decision maker, who should normally be a consultant. Patients should be routinely involved and aware of the progress they are making. Patients (and/or their next of kin) should be able to answer these questions:
- What is wrong with me or what are you trying to exclude?
- What have we agreed that will be done and when to 'sort me out'?
- What do I need to achieve to get me home?
- Assuming my recovery is 'ideal' and there is no unnecessary waiting, when should I expect to go home?
F - Flow early from assessment units. Every ward that routinely admits patients from assessment units should ensure they ‘pull’ the first patient to their ward before 10am every day. This element of the bundle also encourages the ‘E’ of the bundle (early discharge). If discharges on the receiving wards are late, ward teams should consider sitting patients out, transferring patients to the discharge lounge or expediting discharge.
E - Early discharge – a third of patients should be discharged before midday from inpatient wards. The aim is for at least one in every three of the day’s discharges to have left their wards by midday. A simple method to assess whether TTOs are a cause of patient delay on the day of discharge is to ask nursing staff if they have to continually chase them up. If the answer is ‘yes’, it is likely there is an opportunity to improve the current process and facilitate earlier discharges for patients.
R – Review all ‘stranded’ patients (all patients in hospital seven days or more)
Patients should be transferred to their usual place of residence as soon as they cease to benefit from acute care (i.e. have achieved their clinical criteria for discharge) The risk of physical deconditioning and decompensation for older patients increases as each day in hospital passes. At every board and ward round, the following issues should be considered:
- Pharmacy teams should be actively engaged to help reduce delays with TTO processes. Examples of pharmacists helping to improve processes and enable earlier discharges include the introduction of generalist prescribing pharmacists and satellite pharmacies nearer ward areas.
- Early morning ward and board rounds should set the pace for early discharge. This requires teams to prioritise activities associated with discharge, particularly TTOs (medication to take home) and discharge letters, which should be prepared beforehand or during one-stop ward rounds.
- Morning discharges should be the norm. This reduces emergency department crowding and allows new patients to be admitted early enough to be properly assessed and their treatment plan to be established and commenced.
- It is essential for flow that patients are transferred early morning from assessment units. The ‘F’ of the bundle ensures the day starts early and there is space for incoming patients in assessment units that will help reduce emergency department crowding and the associated safety risks.
- Ward teams should be in regular communication with assessment units to agree the name of the first patient they will pull before 10am. The assessment unit teams need to review the patient’s care at the ward or board round and ensure patients are informed beforehand that they will be transferred to the receiving ward at a specified time (before 10am).
- Today is a red day until we prove otherwise and take actions to make it a green day.
- If the patient was seen for the first time as an outpatient or in the ED today, would admission to hospital be the only option to meet their needs?
- Considering the balance of risks, would the patient be better off in an acute hospital or in an alternate setting?
- Is the patient’s clinical progress as expected?
- What needs to be done to help the patient recover as quickly as possible?
- What are the patient’s views on their care and progress?
- A local agreement between health and social care services that packages of care can be restarted, without reassessment, where a patient’s care needs remain largely unchanged. This can be facilitated by implementing a ‘trusted assessor’ model.
- For the majority of patients, definitive assessment of social care needs should occur outside of hospital (discharge to assess).
- The multidisciplinary team should have same-day access to social care advice, ideally at the morning board round, or by phone.
- There should be a local agreement between health and adult social care to share the risk of ‘funding without prejudice’ while responsibility for the long term funding a patient’s care is being established. This will allow assessment to take place outside hospital, ideally at home with support.
- A local agreement by health and social care communities that all referral processes are as simple as possible (i.e. using simple, brief electronic documentation that is quick and easy to complete).
Conclusion
The SAFER patient flow bundle is similar to a clinical care bundle. Many hospitals have found that where the SAFER bundle becomes ‘business as usual’ on all hospital wards, length of stay falls and clinical outcomes improve. To ensure successful implementation of SAFER there are a number of essential components:
- Clinical leadership – implementation and sustaining momentum requires great clinical leadership supported by supportive operational teams.
- Communication – all staff need to be fully briefed and know all the elements of SAFER and why it will help patient flow and benefit patient safety.
- Executive support – senior teams need proactively to support the implementation of SAFER. The active involvement of all members of the executive team is important to success.
- Measurement – all elements of SAFER need to be measured using SPC run charts (statistical process control). All wards should have ‘knowing how you’re doing boards’ to demonstrate their success in delivering the five elements of the bundle
- Social movement – implementation of SAFER needs to be part of a well-managed improvement programme with clear plans and deadlines. A ‘social movement’ needs to be created to win hearts and minds. This involves leaders who are passionate about patient care creating compelling narratives that describe the link between implementing SAFER and improving patient care.