South Warwickshire Foundation Trust took part in a Quality Improvement Flow Programme in the over 75s frailty pathway in partnership with Sheffield Microsystem Coaching Academy and Health Foundation UK. The Key principles of the programme included use of
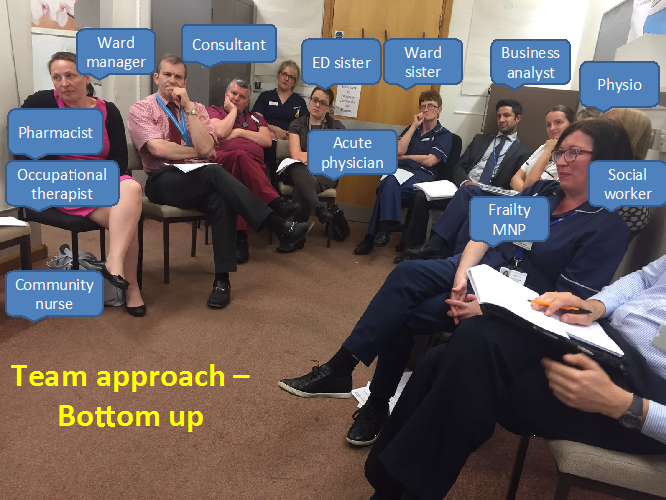
- A bottom up approach including all the key front line stakeholders
- A ‘Big room’ with weekly meetings to form a global aim with use of various improvement and lean tools.
- Current state information to stakeholders with data and patient stories
- Plan, Do, Study and Act cycles to make small changes, and use evidence to measure improvement
- Support to teams with advice, guidance and facilitative resource
The Global Aim:
Over 75s form about half of the medical admissions. The aim was to shorten the Length of Stay (LOS) in a selected proportion of the group -the frail elderly who are identified to need short stay. The aim was to recognise them early, be owned and managed by the frailty team, and discharge appropriately to minimise decompensation associated with prolonged hospital stay.What did the baseline data show us?
- The majority of this patient group attended the Emergency Department (ED)by ambulance
- The self referred attendances peaked between 0900 to 1200 noon and the GP referred patients peaked between 1600 to 1900 hrs
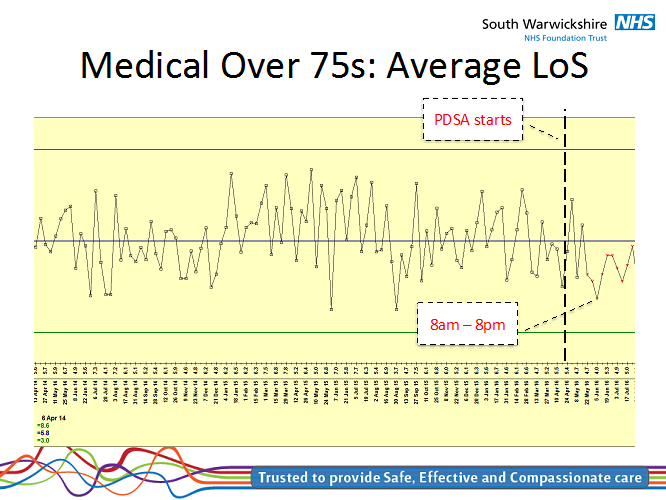
- The average LOS for the medical admissions in the over 75s was 12.5 days
Our Stakeholders:
We had a very wide variety of stakeholders from many professional groups –- The frailty team (consultants, Medical Nurse Practitioners, Occupational Therapists, Physiotherapists, Ward Nurses, junior doctors)
- The Emergency department – consultants and nurses
- The Acute Medicine – consultants, nurses
- The Community Emergency Response team (CERT)
- The paramedics from West Midlands Ambulance Service (WMAS)
- The General Practitioners with special interest in frailty
- Support from South Warwickshire CCG, GP federation and Trust management
Process mapping using patient stories:
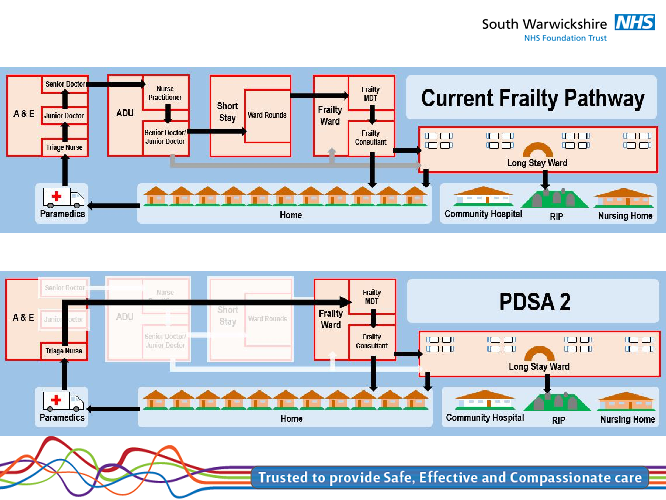
Patients were conveyed to the ED by the paramedics, seen by the ED triage nurse, the junior and senior medical team, and referred to the on call medical team. They were subsequently seen by the junior and senior acute medical team and referred to the frailty team almost a day or more after arrival. Often the management plan needed to be changed after the Comprehensive Geriatric Assessment (CGA) was done.Many of the patients who missed being seen by the frailty team were admitted in peripheral wards and their LOS was even longer.
Value Stream mapping:
The team decided to remove the non value added steps in ED and Acute Medicine in the current pathway, take and retain ownership of the patients from the point of nurse triage in ED for the pilot.
Reason why frailty team has the best impact:
They take time to complete the CGA, which teases out the exact needs of the patients and helps implement the appropriate management. The ED and Acute Medical teams do not often have the time, expertise or the motivation to undertake this.Results:
- 63% of patients were discharged from ED, AMU or Frailty to the destination they came from with an average LOS of 2 days
- 23% whose ownership could not be retained with the frailty team and had to be moved to peripheral ward had an average LOS of 10.5 days
- There was a significant improvement in overall LOS in over 75s in medical beds with 13 consecutive data points below average on the run chart.