So we thought you might like to hear about our experiment that has been coproduced between patients, primary care staff, ambulance staff and emergency room (ER) staff in Jönköping County Region. Our scheme is the first of its kind in Sweden.
The starting point was a consensus that the current ways that county residents search out and utilise healthcare services to meet their immediate health needs was not optimal. There was confusion about the role of the primary care centre and the role of the ER. As a result, patients didn’t always get appropriate care and we didn’t make best use of our health and care resources in Jönköping County Region.
Over the previous four years there had been four significant attempts to improve the situation but none of them delivered sustainable reductions in the numbers of people attending the emergency room. These included initiatives to improving the flow of patients coming to the emergency room through better connections with orthopedics, medical and surgical departments; information campaigns aimed at patients and a test to locate a District Nurse in the ER to take care of primary care patients.
We realised that we needed a more systematic approach. In Jönköping County Region we have a tradition of bringing patients and staff from across the health and care system together to solve problems. There is a “myth” in healthcare that if a patient arrives at the ER, they should be treated at the ER, even if their care needs would be better met in primary care. The consequence of this is that the pathways for patients across the system will never be clear and never optimal for the people getting care. So we created a codesign project with patients, staff from primary care, staff from the ambulance service and staff from the ER to see what is possible. We started in May 2016.
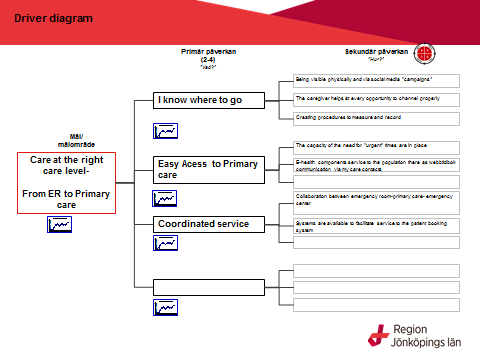
Mission of the project: To change patient flows and patient search patterns from ERs in the county so that primary care becomes the first-line choice for patients. Goal: To reduce the number of ER visits by 15% during the day Approach: To seek to identify, segment and test new methods and approaches involving both patients and staff across the system to change the patient flow, in a way that benefits patients.
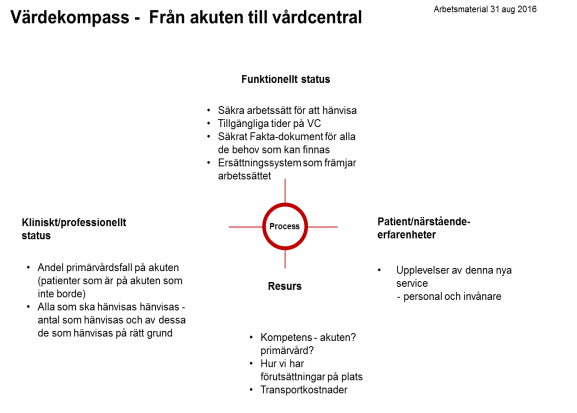
From May to September 2016, we assembled the data and co-designed the new flow with the patients. We clarified the mission of urgent care services within primary care and clarified that the ER is for people with serious illnesses, accidents and life-threatening conditions. The data demonstrated that it was possible to show patients the route from the ER to primary care and that the pathway from ER to the best environment for care could be controlled effectively if the right systems and support structures were in place. The data further showed that it was often young people and people with young families who came to the ER but who would benefit more from primary care.
Previous attempts had largely been about activities within the ER but in this project, there is much broader participation. For instance, we have co-developed procedures with the ambulance service so that only patients with serious illness, accident or other life-threatening conditions are taken directly by ambulance to the ER. The ambulance crew will take all other patients who need treatment to the primary care centre. Over time, we envisage that ambulance crews will take more patients to primary care centres than they will take patients to hospital. Already during 2016, we have seen a significant change, with 25% of ambulances now taking patients to primary care rather than the ER.
Our new way of working
When patients come to the ER who should be treated in primary care (in line with the guidelines and protocols of the Region) we follow a different process than was the case previously. The nurse in ER phones the primary care centre that the patient is listed with to say “we are sending a patient to you with these problems.” The simple rules are:
- The ER identifies the patient and the primary care centre welcomes the patient the same day (sometimes the appointment is for the next day but nearly every patient who wants a same day appointment in the primary care centre gets one)
- The ER team book the appointment in the primary care centre and the patient leaves the ER with a definite primary care appointment at a time that suits the patient
- If required, the ER team will book and pay for a taxi for the patient to get to the primary care centre
The experience so far
In terms of patient experience, most people are very satisfied about being taken care of in primary care. They report that they have received a high standard of care and informed where to go next time.
The people who are transferred from the ER to the primary care centre are most commonly seeking care for virus infections, skin problems, minor wounds and anxiety. In terms of next steps with our patient population, we need to segment young parents and help them with navigation of the system. In addition, three primary care centres are currently analysing the data around people who frequently visit the ER to see how they can be supported on a more proactive basis.
Originally we were sending an average of five people per ER to primary care each day. We expect this to rise to 15 per day.
After we extended the daily hours for the experiment in February 2017, the numbers of people being transferred from the ER to primary care rose significantly.
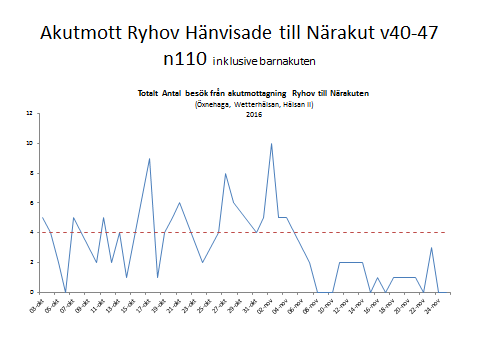 Numbers of people from ER to primary care
Numbers of people from ER to primary care

February
We are seeing the proportion of people who visit the ER but don’t get admitted to hospital increase:
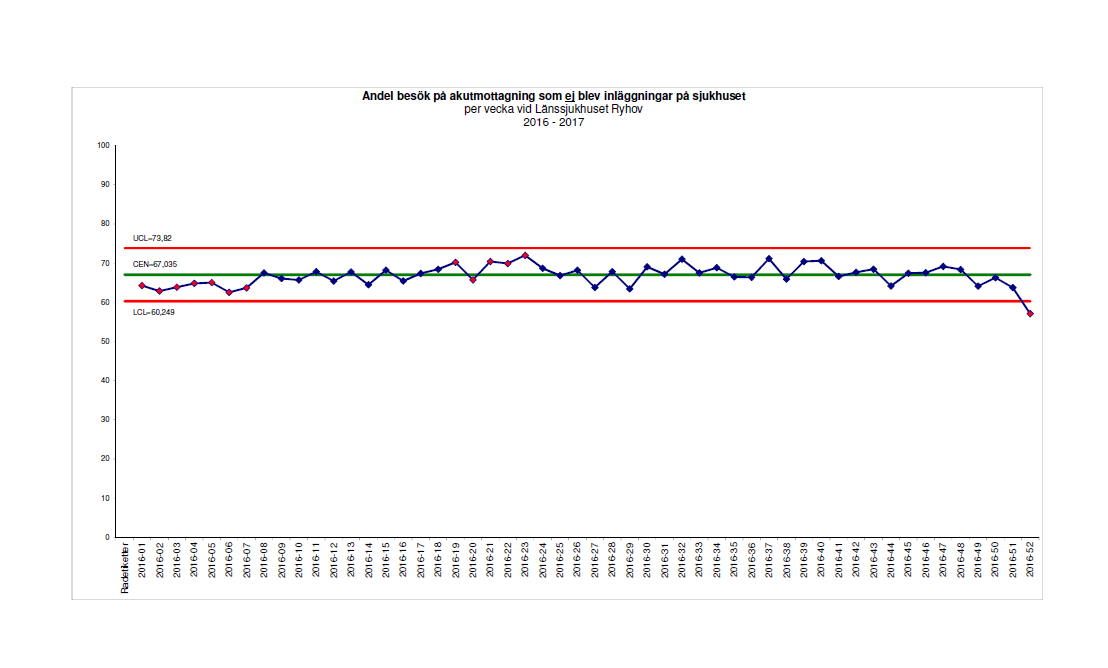
We are learning greatly and the early data suggest that our project will meet its goals.
We have learnt that the heart of this project is creating trust and building the relationship between ER and primary care. It has been helpful to have a systematic approach, collecting stories from patients and coworkers and having meetings to analyse and reflect on how we are doing. We give the teams excel spreadsheets for measurement and an opportunity to take part in a call in every other week. There are lots of challenges, and much more to do. For instance, the nurses in the ER still find it difficult to send patients to primary care, feeling unsure if they are doing the right thing.
Here is a short film about the coworker experience (sorry that it is in Swedish) https://vimeo.com/191646400/80739acd11
We have been able to engage our General Practitioner colleagues on a large scale by starting the experiment on a small scale. The first three primary care centres that took part were able to report a positive experience. We have learnt that we need to improve capacity in primary care during the daytime. Sometimes, primary care centres tell the patients to go to “primary emergency centre” after office hours because they don’t have any time slots available for them during the day. This remodeling of primary care fits with the wider strategy of Jönköping County Region to extend the role of primary care in wellness, prevention and population health.
We also need to use E-health and online booking on a larger scale than we do. From April 2017, people living in Jönköping County Region will be able to book slots online at the “primary emergency centre”. Hopefully this will help people to choose primary care instead of ER where it meets their needs.
We have learnt that we have to come together as a system to support the flow of services around the needs of patients. Next we have to spread this approach to the whole of Jönköping County Region.
Contact: Pernilla Söderberg Development Leader
Qulturum, Jönköping County Council
Email [email protected]
Twitter @pernillasoderbe

