The concept of the Longest One Waiting Vehicle, LOWVe, came from a long serving member of staff who was becoming increasingly concerned about the increasing length of time we were taking to get to patients, the secondary effects this was having on these patients conditions and the types of patients this was affecting.
Often patients that have a lower categorised call are older, frail or socially isolated members of our community. Our member of staff, Steve an Ambulance Technician, was becoming gravely concerned that we were failing these people. He started to speak about these concerns and the idea that maybe an alternative method of looking at the problem was discussed.
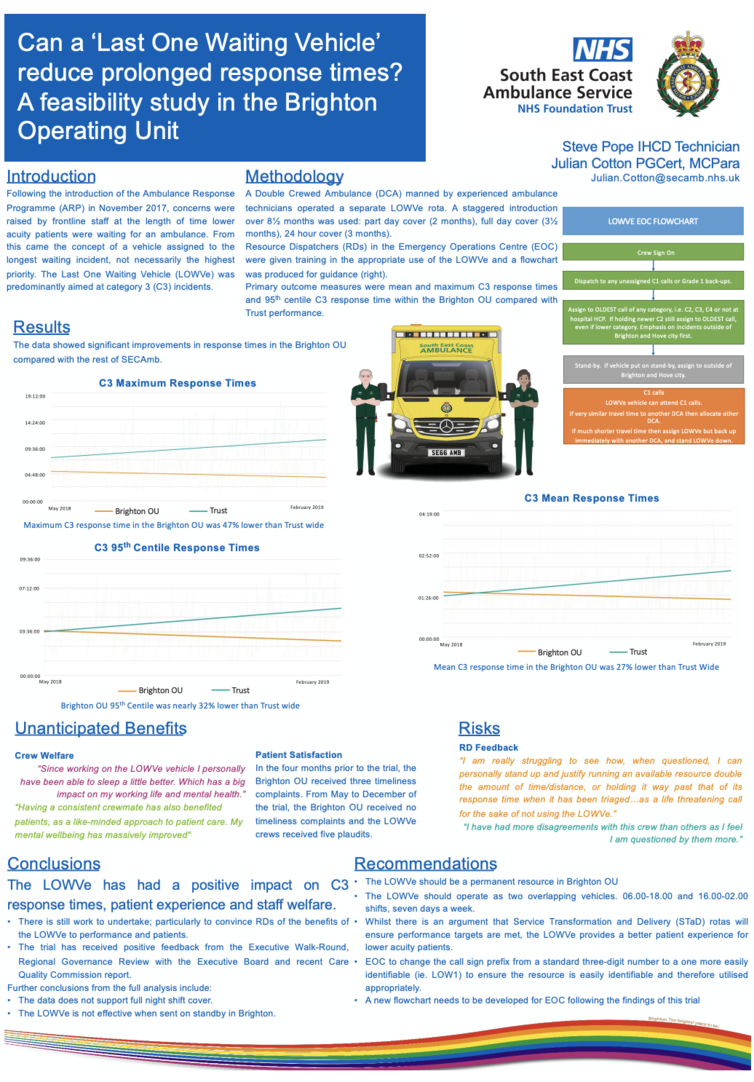
Traditionally ambulance services respond to patients with highest acuity first, then work down the list of calls until all are covered. If another higher acuity call comes in then the lower acuity call has to wait. This concept works fine when the number of resources is greater than the demand. But locally and nationally ambulance services have been dealing with a continual year on year increase in call volume, a growing and ageing population and a society that wants a more instant access to the NHS.
The idea was to have a vehicle that worked from the bottom of the list up. So instead of defaulting to the highest acuity call, they would attend to the oldest call on the system regardless of call category. Whilst the rest of the ambulances in the area would work to the normal method of highest acuity first. It was hoped that with the addition of the LOWVe vehicle there would be a marked reduction in the longest time patients would have to wait.
After discussion it was felt that for the trial the vehicle would be manned by experienced Ambulance Technicians rather than paramedics. They were all well practiced in patient assessment, had a good knowledge of alternative pathways available locally and happy to call for higher clinical assistance if required.
For governance a Standard Operating Procedure (SOP) was written and presented to Clinical Innovations and Service Change Group for approval, which was given. This SOP also contains an easy to follow flowchart for EOC.
Several visits to EOC were undertaken, as well as email correspondence, to advertise, inform and educate the EOC staff. This was very important as the concept requires the RD’s to operate in an unfamiliar way. The RD’s change which dispatch desk they are working on a daily bases so this process was repeated several times.
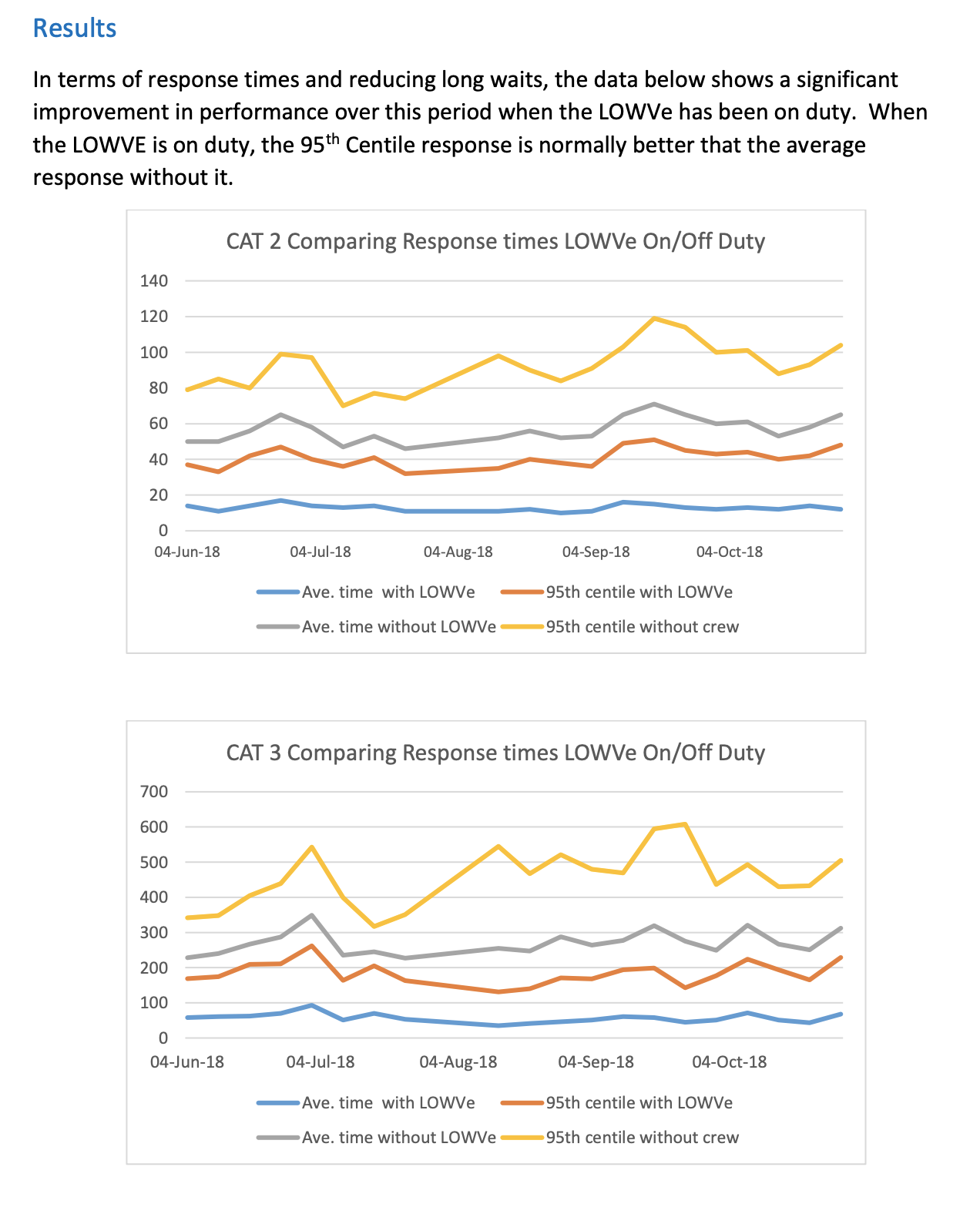
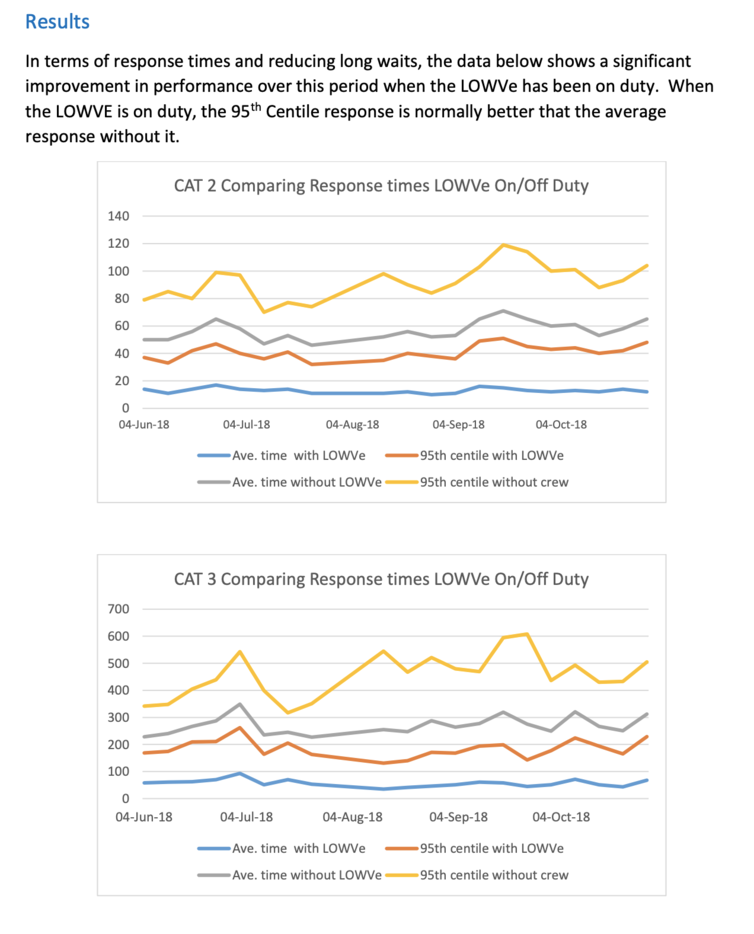
The trial took place in three stages, and successfully reduced long waits for ambulances.
You can read the full trial report here