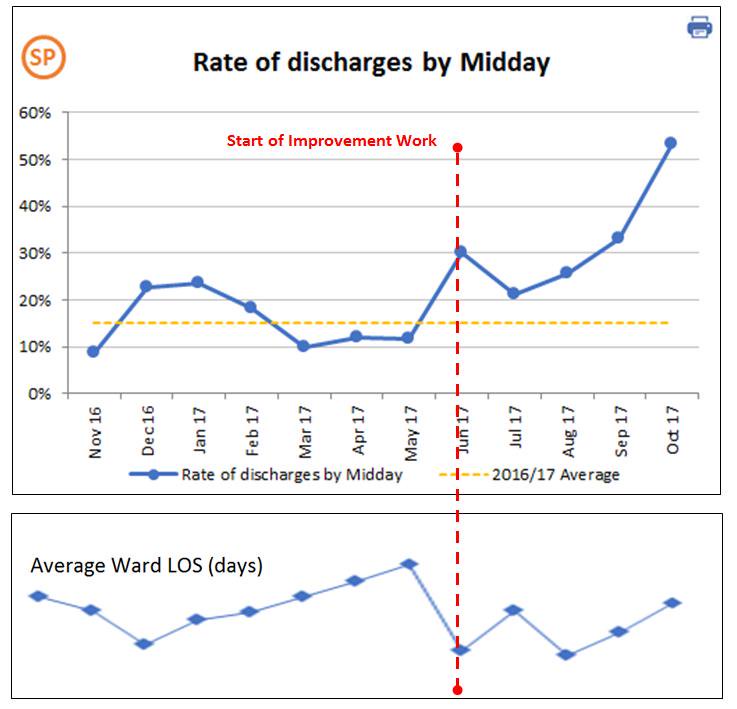
On the face of it, this adds a night to the patient’s stay. However, the proportion of patients discharged before noon has increased and our ward now performs best on this parameter of all the wards in the Trust. The length of stay has either remained the same or decreased, rather than the expected increase. The ward nurses have found several advantages to this process and fully support it. For example the early bed vacancies allow early transfers up from the Emergency Floor (EF). This means a less disturbed night for all the patients and a reduction in workload for the night staff that are often very pressed for time.
The idea came to me from thinking about Flight Departures at an airport. Flights are not vaguely planned for “Thursday”, but for Thursday at a very specific time. The passengers know that they have to prepare everything in advance and be in the correct place at the correct time to depart to their destination. The airline is fined if the flight is importantly delayed, so the planned and actual departure times are monitored carefully.
Why is the length of stay not increased, by seemingly keeping the patient in longer? Firstly the departure is more secure. Our juniors had started asking for 6 a.m. bloods to be sure a discharge was safe. I argued that either we did not need the bloods, or if we were that insecure about discharge, we should not rush. Sometimes, as on the M25 when it is busy, flow can be increased by slowing the traffic down. Also if we are still preparing the discharge of a patient with complex needs on the day of discharge it is bound to be late in the day when the patient leaves. This can be awkward for the care agencies that are likely to be involved in care of patients with complex needs.
The more important factor turned out to be something unanticipated. If the bed is vacated by 9 a.m. it can be ready and filled at 10 a.m. In this way the next patient from the Emergency Floor can be seen at the end of the morning ward round. If that patient had arrived after 4 p.m. the first time we would assess the patient would be the next morning. Seeing the patient earlier allows for refining or correcting the diagnoses and management plans. Perhaps more importantly it allows the doctors and nurses to assess the patient, to more confidently answer, the next day, what progress the patient has made. Answering “Is the patient getting better?” is a complex process, and depends a lot on seeing the patient at least twice. I believe one of the reasons that a ward move adds a day to the length of stay is simply that the first time the doctors see a new arrival it is hard to answer “Is the patient getting better?”. Once we know that the patient is getting better, we can more confidently plan the discharge. The seemingly “added time” is recovered by buying back time by seeing the new arrivals nearly a whole day earlier.
Actually I believe we do not often add a night to the stay, the impact comes from the Consultant setting the Scheduled Departure Time. It is a small change to say “You will be discharged at 9 a.m. on Thursday, and if necessary you will go to the Discharge Lounge” from “You will be discharged on Thursday.”
We have learned other lessons:
Our nurses have seen that this makes for quieter nights for patients and staff. All our nurses rotate onto nights so they know that they are helping their own colleagues by being busier in the day time. Our nurses are enthusiastic for on time departures and to get the next patient early. On occasions they go down to the Emergency Floor to hunt for patients and bring them up to the ward. This helps the EF, because they do not lose a staff member on a transfer. If you have unenthusiastic staff, the idea is likely to fail!
Our nurses are also at ease with an early morning nurse Led discharge, without the need for a doctor’s review. The nurses do not need a lot of documentation as they do at weekends for nurse led discharge, and simply trust our word. In turn we trust the nurses to abort a departure if necessary. Early on a patient had a fever of 38.5C, and the nurses called the departure off. Mutual trust in professionalism matters.
Our doctors can work on the discharge notification and medications on the preceding afternoon, so that the quality of the summary is improved and the “TTO” prescriptions are not subject to last minute lengthy delays.
In recent days we have started to run into a new problem. The bed, once vacated, may stay empty for 12 or even 16 hours despite the hospital being in “Business Continuity” and messages being sent out to “Prioritise Flow”, as we fail to meet the 4 hours target. There is a problem about getting patients off the EF and up to the ward. This probably reflects the EF staff being over busy, and unable to identify, release and transfer suitable patients in the middle of the busy morning’s work. In our Trust we are also poor at ensuring that patients are transferred form the EF to the most suitable ward care team e.g. make sure a patient with ascending cholangitis is transferred to a gastroenterology ward. I believe we could improve at early identification of these “Speciality cases” and then accelerate them to the speciality ward, maybe even without a Consultant post take review, if the transfer could be done at 9 a.m. on a weekday. I believe a doctor of registrar grade can identify patients who need specialist downstream care. The night medical registrar could identify a case of ascending cholangitis and mark the patient for priority early transfer to the gastroenterology ward. I suspect we are also short of porters and other staff essential to timely transfer e.g. ward clerks. In our Trust we get no backfill for ward clerk’s leave. There is a lot of administration and filing work involved in a transfer from EF to the ward, and in the absence of a ward clerk it will be a Nurse or Doctor who does this work, bleeding away their time for patient care.
The worst times for blocked flow are immediately after bank holidays, particularly if Christmas falls at a weekend and at Easter, which always involves a “four day weekend”, yet still seems to catch the NHS by surprise every year. Outside of emergency department the staffing levels for doctors on the wards on bank holidays are at weekend skeleton crew levels. For example Christmas 2017 involved 4 consecutive days of skeleton crew levels of doctors on the wards. Nursing levels do not reduce for bank holidays, so why should doctors? I went in on Boxing Day and New Year’s Day to do ward rounds on our general ward. I was “Solo” without any other Doctor to help (nor a nurse or pharmacist), whereas on my ordinary working days I will have at least one Junior and see 13 cases. On those days I saw 27 cases by myself. Each day I did at least an hour’s work filing clerking sheets and results into the notes in order, because our ward clerk was on leave. I managed to discharge at least 2 patients each of those days – 2 cases that could be crucial to flow and hitting targets. With just one junior doctor, we could have discharged earlier in the day. If it had been the usual staffing level of 2 consultants and 2 juniors and a ward pharmacist present, we could have discharged even earlier and probably have accelerated care of all the other patients. It would seem a small change to me that Doctors would be expected to work bank holidays and then get the worked days credited to their annual leave allowance. Maybe we could move that way by ensuring every team had one ward round on bank holidays, supported by at least one junior. So to use our ward as an example, instead of the usual weekday rounds of 2 consultants with at least 2 juniors, we could ensure one round with one Consultant and one junior. The support of a full team of therapists and pharmacists would also be essential for safe discharges on a bank holiday. For example on New Years day there was a patient who could have gone home if he had passed a physiotherapist’s stairs assessment.
Sometimes it may be helpful to schedule a discharge for a bit later in the day, and then this could coordinate with, for example, a planned step down of a patient from intensive care.
This idea of setting a scheduled planned departure time from hospital feels to be going well and the early evidence supports that feeling. It is a simple idea, that maybe you could adapt and try in your organisation?
Dr Gordon Caldwell - Consultant Physician Western Sussex Hospitals NHS Foundation Trust
@doctorcaldwell