Leadership at all levels
This journey has been built on clear and consistent leadership at a senior, strategic level and at an operational and frontline level. This has been critical to enabling people to focus on the patient and keep two simple questions in mind at all times regarding discharge: Why not home? Why not today?
By keeping these in mind, problem solving has been focussed and responsive with agencies pulling together to find a solution rather than looking to blame different parts of the system. It has allowed innovation to flourish. Crucially a ‘can do’ culture has emerged, with different agencies all rising to the challenge as the bar has been pushed higher by our frontline leaders. A key early exercise, which helped to establish a sense of common purpose as well as operational understanding of the barriers to discharge, was a joint “walk the wards” programme including commissioners, community health and social care providers and acute trust management and ward staff.
Transparency
The Better Care Fund (BCF) gave Leicester a platform to drive forward an existing local ambition about integrated care. The starting point was inclusion and transparency – putting the available resources and what that resource delivered onto the table in an open and honest way. This enabled all stakeholders to engage in a debate about how we used what was available to make a difference. Included in this approach was seeking collective agreement about the data from the outset, so that subsequent discussions avoided the usual pitfall of debating the accuracy of numbers rather than the problems to be resolved.
During the life of the BCF, annual challenge meetings have engaged commissioners and providers to review the investments and the outputs / outcomes and agree the next year’s programme of activity to be funded by the BCF.
Flexibility
Challenges to both timely discharge and effective admission avoidance have developed and changed; as one issue is addressed, a new one emerges and needs a different solution to those initially planned. Both leadership and transparency supported rapid cycle testing and changes.
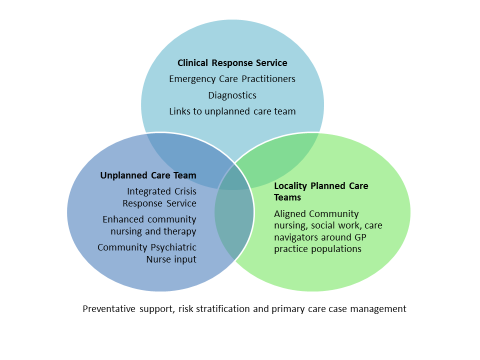
Some practical examples were the change of focus for the Clinical Response Team, to pick up care home support, which proved to be effective in avoiding admissions but was not part of the initial plan. Another example is the in-year extension of the work of the Integrated Crisis Response Service to include the pre-admission areas of the acute hospitals, evolving from what was a community brief at the outset of the plan.
Results
There is more to do and challenges persist but the trajectory is right. Leicester was reported to be the third most improved area for Dec 14 – Dec 15 with a reduction of 46.3 % on delays.

Author - [email protected] - Director, Adult Social Care and Safeguarding