#Red2Green bed days are a visual management system to assist in the identification of wasted time in a patient’s journey. It is most applicable to in-patient wards in an acute hospital setting. At the centre of this is the person receiving the acute care whose experience of that delivery of care is one of total involvement and personal control with expectation of what will be happening. One of the key principles of Red2Green (R2G) is ‘doing today’s work today’. This has relevance for all professional and managerial staff working with patients day-to-day. A critical component is identifying constraints and working together to find local solutions to address them.
Background
Within Chesterfield Royal Hospital Foundation Trust (CRHFT) the initial response to #Red2Green days was to establish a R2G lead team for the organisation. It was identified that to have the greater benefit R2G would be aligned with the ongoing transformation of the hospitals discharge teams and the discharge to assess processes.
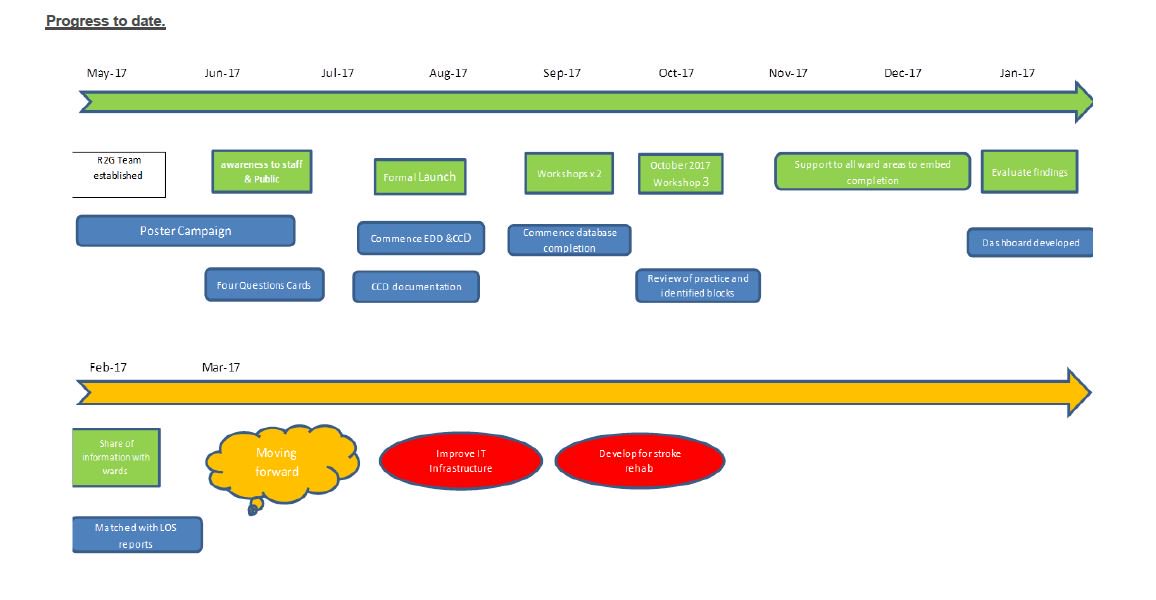
During May 2017, one whole time equivalent band 6 Nurse and one band 3 HCA were employed to support the discharge team with the introduction and roll out of R2G to all adult in-patient wards within CRHFT. The R2G nurses attended masterclasses delivered by NHS Improvement, underpinning knowledge and providing support to establish R2G throughout the trust.
Clinical leads were identified from medical and surgical divisions along with therapy leads prior to commencement of the project. This ensured that a multi-disciplinary approach was established for implementation.
A project plan and a timeline for implementation were developed with the whole team and this was shared with the hospital leadership team. Senior support for the project was positive with an executive lead for the programme identified.
It was discussed in early project planning meetings that to promote success the focus would primarily be improving patient care, with operational improvements to patient flow being a secondary positive outcome for the trust. The initiative was thus titled Patients’ Time Matters. A poster campaign was commenced utilising resources from NHS Improvement to introduce the concept of R2G throughout the whole hospital. Patient credit cards were developed and introduced; ensuring early participation of patients/relatives providing them with the 4 key questions.
The initiative was formally launched in August 2017 across the whole trust. A launch presentation was conducted by the R2G team and medical lead to all staff. At this event all in-patient ward Matrons were presented with a timetable of education workshops in place for their ward teams.
The process was introduced through three different stages. Before each stage a workshop was held to discuss and educate staff and also to support with any specific changes that could be made to help the process fit the individual specialities.
Progress to date
It was planned to launch the initiative to all hospital wards in “one big bang”. Having only a very small implementation team and due to the size of the challenge, a plan was put into place to roll out the programme in 3 stages. This allowed the R2G team to lead workshops with each ward team prior to each stage, supporting consistency of the process throughout the hospital.
All workshops were well attended by nursing and therapy staff, though challenges continued with recruiting engagement from senior medical col-leagues. A Clinical Criteria for Discharge (CCD) form was developed with support from multi disciplinary teams (MDTs) and introduced for each patient in an attempt to engage all doctors within the trust.
Success of the forms use was variable though the discussion of CCD was now evident across all areas even if documentation was in different formats. A decision was taken that it would be acceptable not to utilise the CCD forms, if it was clearly evident that a CCD had been discussed and the MDT team were aware of the criteria. Following workshop 1 the first stage of the process was launched. Daily ward huddles of the ward MDTs were in place ensuring a senior clinician review of each patient with a transparent EDD and CCD in place.
Two weeks following stage 1, Workshop 2 was commenced again led by the Red2Green nurse for all the ward teams. At this stage the electronic database for monitoring R2G was introduced. There was awareness that this potentially would involve an added task for nursing staff completing the database. This proved not to be an issue and ward teams were enthusiastic meeting this challenge.
Compliance with completion of the database and understanding of the process was mixed across all areas, requiring regular support from the R2G team. The data that was extracted regarding compliance was used by the Red2Green nurse to identify where added support or training may be required and to engage areas showing less engagement. It also identified that weekends were a particular problem for the process due to staffing levels and reduced members of ward MDTs, resulting in the database being incomplete for these days. Following introduction of stage 2 the R2G team continued to work with all ward areas to provide education and support.
One month after the launch of stage 2 workshop 3 was held. Workshop 3 was commenced to review the process and to receive feedback from all ward areas. At this stage the ward teams were very keen to see results of R2G. Unfortunately the R2G team were finding difficulties collating all the information gathered into meaningful data.
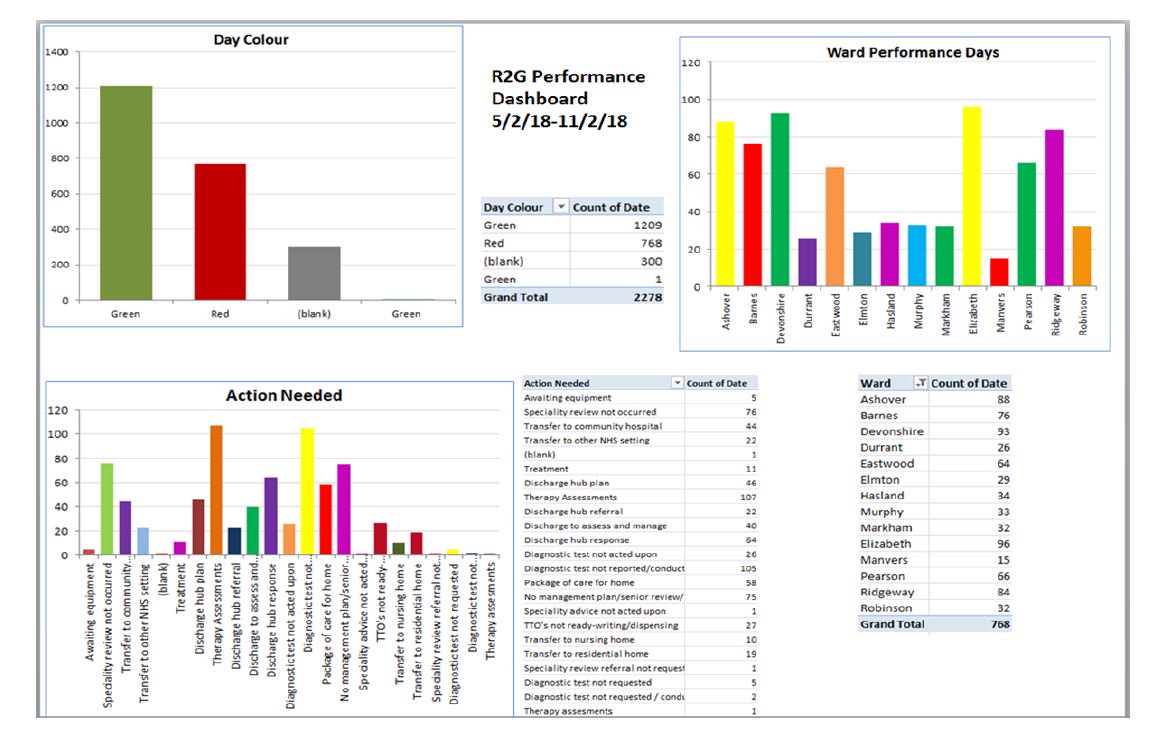
By the end of December 2017 early January 2018 it was possible to produce a weekly dashboard of the previous week’s data. This was made available for all wards to view and presented to the executive lead.
What we have produced
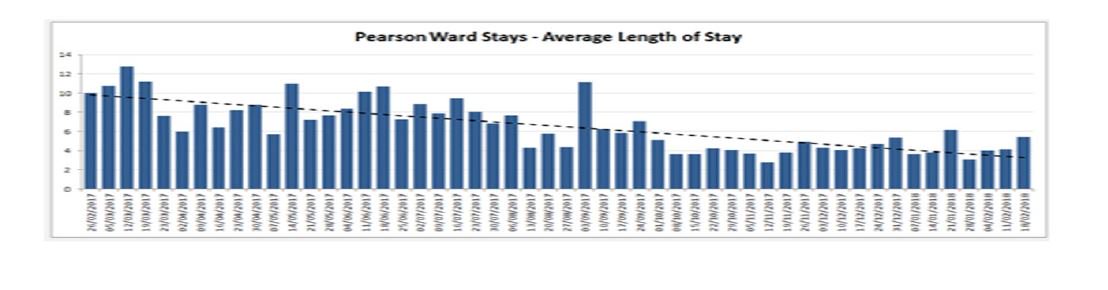
We are now in a position to provide weekly updates to each ward and for the trust as a whole in the form of a dashboard. The report identifies the number of red days and green days reported for the ward with a breakdown of the red day actions that were not completed. For the trust dashboard ward performance data is also added, identifying participation of each ward, which is continued to be utilised to provide extra support to the ward areas by the R2G nurse. We are able to provide data on an individual patient basis though this is presently very time consuming using the established data base. The length of stay for each ward and for the hospital is also matched against the commencement of the R2G initiative. Results demonstrate that areas with a higher level of participation with R2G are producing a greater reduction in LOS.
Conclusion
The Red2Green process has been successfully introduced across CRHFT. Although results highlighted by the dashboard are not consistent across all areas, there is a definite increased awareness of patients’ needs and wasted time for patients within the acute trust. This has resulted in supporting a reduced length of stay for patients and earlier identification of patients not requiring to remain within an acute hospital bed at an earlier stage.
The process required involvement by the whole MDT and a joint understanding of the patient’s needs. Success was achieved by early involvement of all teams and communicating patient stories to them prior to launch of the process. Midway through the project a discharge week was held at CRFT. During the week different teams were asked to focus on a particular area of their choice to try and make a difference. Therapy teams focussed on #EndPJparalysis and keeping patients active, our community colleagues attended to promote Discharge to assess processes and our adult care supported with education to all trust staff. Continued events maintained awareness and enthusiasm and supported success of the initiative.
Initial findings are that the present database does not suit CRHFT stroke rehabilitation patients. Further work is to be undertaken with the stroke MDT to develop an individual process that will be effective for this group of patients.
It was also found that wards that employed a dedicated discharge co-ordinator, demonstrated an increased performance with a more robust process for managing R2G. These areas demonstrated a reduced length of stay.
Next steps
The aim is for the R2G process to become the daily norm within all in-patient ward areas. A review of the Red day actions is to be reviewed to under-stand if there is a need to extend or simplify the reasons for delay. Presently the R2G nurse is investigating red day reasons reported and finding high levels of discrepancy.
There is a vision to simplify the data collection and incorporate R2G database with the trusts chosen bed management system and reduce duplication of the nurse’s workload. The present electronic database presently in use for recording R2G days only provides limited ability for providing beneficial results and data that can be utilised to make a greater difference to patient care. The continuation of the project will primarily be to establish an IT solution to these challenges along with customisation of the process to suit all clinical areas. Different IT systems reviewed do offer remedies to many of the issues with the next steps to work closely with CRHFT IT teams to support infrastructure transformation .
The vision being to visualise in real time the progress of each patient with the goal of eliminating wasted time throughout their care.
CRHFTs #Red2Green aim will continue to be that Patients’ Time Matters to us all
Warren Hutson - Lead Discharge Nurse Chesterfield Royal Hospital - [email protected]
