
Introduction
It is recognised and accepted that there is a need to support the wider health economy, and for the Health and Care Trust to play a part in ensuring flow across the whole system in Worcestershire, as well as ensuring the best patient experience and outcomes.
With an increasing demand on urgent care, downstream flow into Community Hospitals has to be available for those patients that require care (step down) into a bedded facility from the Acute Hospitals. There also has to be the capacity to enable an alternative option for GPs and the Enhanced Care Teams to admit to Community Hospitals (step up) as opposed to a referral to Acute Hospitals as admission avoidance. A new strategy around transforming Emergency care with a key theme of the right care, in the right place at the right time is the drive to ensure that there is capacity in our Community Hospitals.
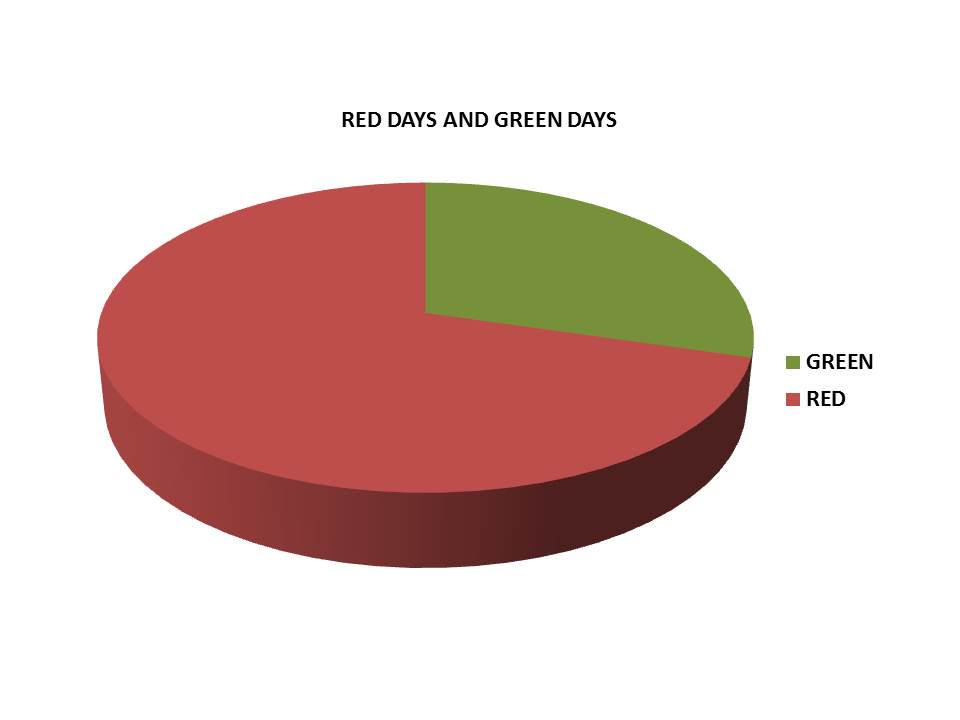
Dr Ian Sturgess (NHS Improvement) has developed a visual management system of Red and Green days. The philosophy of this approach is that the experience of a non value day adds to a poor patient experience, delays the patients’ progress in recovery and creates an unnecessary longer length of stay. A Red day is a day when a patient is waiting for an action to progress their care or that an action could have been carried out in another setting. This was the basis of the audit carried out at Tenbury Community Hospital.
How the audit was carried out
At Tenbury Hospital 17 inpatients notes were reviewed utilising the Emergency Care Improvement Programmes Red and Green days approach. The 17 sets of patients’ notes were examined to identify the total number of Red days that each patient experienced. The patients’ admission date was noted and the number of days in Tenbury hospital identified up until and including the day of the audit. The referral source was recorded, as this would indicate if the patient had already had a period of an in hospital stay if stepped down from the Acute Hospitals. Red days were recorded regardless of whether the patient was clinically stable or not, as such days would indicate there had been no valuable action. The Green days recorded were days when there had been an action or an action had occurred that was going to impact on the patients care or progress their discharge e.g. Therapy or clinical investigation and/or a change to treatment. The total number of days reviewed were 79.
The results
The results indicated that almost 75% of the total number of patients’ days were red days. The impact of certain pathways did compound this; one patient referred as a Plaster of Paris patient (POP patient) and another admitted whilst waiting on a date for Surgery at Birmingham Hospital as a step up patient.
There were three significant outcomes of red days:
- No access to or continuity of rehab goals over the weekends.
- Waiting on families to attend MDTs or make decisions re: their relatives’ on-going care.
- The greatest number of bed days lost was due to waiting on going long-term care, further exacerbated by two patients living outside of the county.
Conclusions and recommendations
- There is a need for seven day Therapy support or an alternative to ensure that the prescribed rehab program continues over the weekend.
- Escalation to managers to support out of county delays
- Setting expectations and ensuring robust setting standards around family engagement and progress meetings.
