Making sure patients drink enough can have a big impact on illness and falls, so for this reason, a hydration project was launched at Hawkhurst Hospital.
It involved raising awareness of the importance of patients drinking adequately while they are in hospital, in the hope the good habits will continue when they go home. The project also included colleagues having additional training and a hydration champion being appointed.
The work has been so successful, Kent Community Health NHS Foundation Trust, will now share it with all of its community hospitals .
One patient to have benefitted is Derek Wells, 68, from Tonbridge, who during his stay at Hawkhurst Hospital, had many visits from healthcare assistant and hydration champion Joseph Bridger.
Derek said: “Joseph looked after me and kept telling me I needed to drink more. He’s up and down the corridor all the time and brings me water, squash and cups of tea.”
Another patient, Alan Hyde, 83, from Snodland, said: “They’re very good at the hospital. They bring me lots of drinks and tell me how important it is to drink, to help me get better.”
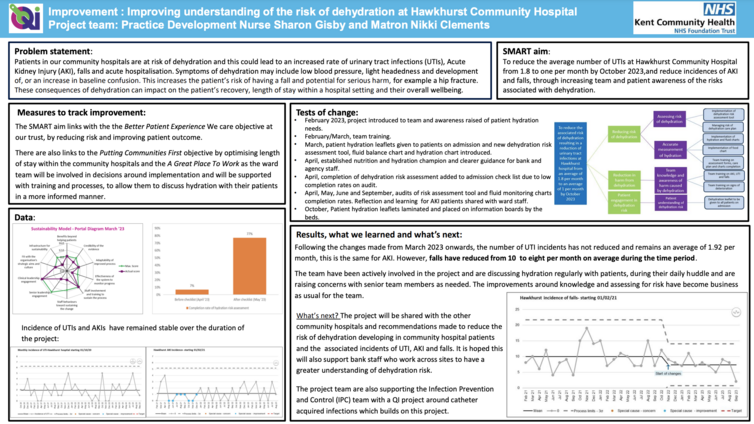
The work was led by Practice Development Nurse Sharon Gisby, with Sharon’s quality improvement (QI) project supported by Matron Nikki Clements and the team at Hawkhurst Hospital. The aim was to increase awareness of good hydration monitoring on hospital wards, with the aim of reducing falls, urinary tract infections and acute kidney injury (AKI). Sharon hopes that in the long run, the work will also reduce the numbers of people who have to be re-admitted to an acute hospital with complications associated with dehydration.
Sharon said: “Not drinking enough can lead to dizziness and for older and vulnerable people to falls and fractures and other complications associated with dehydration. Older people often need extra encouragement to drink enough, because they don’t always feel thirsty. As we get older our thirst reflex is not so effective, but we still need adequate hydration. Patients may also forget to drink if they have a cognitive impairment.
“Older people can sometimes stop drinking in the evening, as fear they’ll be getting up to use the toilet several times during the night, but if they drink less, the bladder can become irritated resulting in them needing to go to the toilet more. They may also be more vulnerable to developing a urinary tract infection, becoming confused and more prone to falls and fractures.
“In hospital, sometimes patients don’t want to drink if they need assistance to walk to a toilet. They don’t like to ask a member of staff for their time and help, but that is what we are there for. We are more than happy to help.”
The project has involved introducing a new a dehydration risk assessment tool, which Sharon has developed alongside new hydration and fluid balance charts. Patients are encouraged to read a healthy hydration patient leaflet and fill in the hydration charts themselves, if they are well enough. These remind patients to drink at least eight cups of fluid a day, ask them how many times they have been to the toilet and the colour of their urine.
Sharon said: “Acute Kidney Injury (AKI) is a good indicator that something more serious is wrong, therefore should be recognised and treated quickly as it carries up to a 30 per cent mortality rate. Whilst it is recognised that AKI has many different causes, good hydration practices may go some way to preventing it in some cases.’’
“So far the results are encouraging. We have seen a reduction in falls, on average of two a month, while UTI and AKI numbers at present remain stable.”
Colleagues have welcomed the new fluid monitoring charts and reported how much clearer and easier to use they are then the previous charts. They have been involved from the start and been given opportunity to help guide the project’s progress.
Improving-understanding-of-risk-from-dehydration-at-Hawkhurst-hospital-A3-FINAL-pdf.pdf

