The Merseyside Impaired Glucose Regulation pathway (IGR) is designed to prevent or delay the onset of type 2 diabetes for those at highest risk by the identification and management of IGR (Otherwise known as non-diabetic hyperglycaemia).
Identification of IGR supported by evidence based lifestyle interventions represents a significant opportunity to prevent or delay the onset of Type 2 diabetes.
The pathway, guidelines and supporting materials are evidence based and freely available. For access to full guidelines, patient information material and a range of other resources please use the link below. http://www.cmscnsenate.nhs.uk/strategic-clinical-network/our-networks/cardiovascular/within-network/diabetes/
IGR can be described as blood glucose levels above the normal range, but below that required for a diagnosis of Type 2 diabetes. Those with IGR are 5 – 15 times more likely to develop Type 2 diabetes compared to people with normal blood glucose. Without intervention the majority of people with IGR will develop Type 2 diabetes within 5-10 years. For those people at highest risk of developing Type 2 diabetes evidence suggests modest lifestyle changes can delay or even prevent the onset of diabetes.
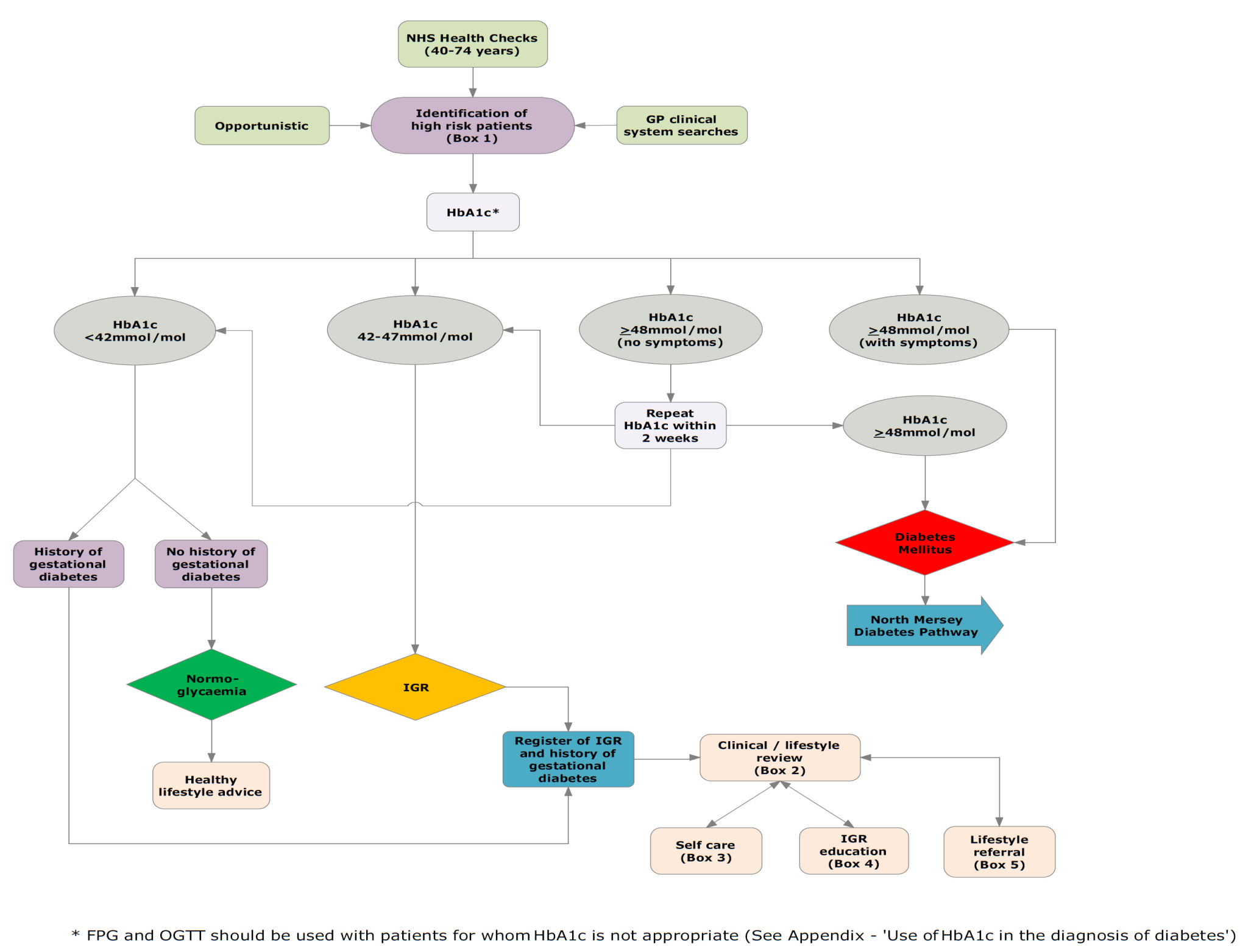
Pathway overview The pathway is initiated via the NHS Health Checks programme or opportunistically in primary care. Identification is usually via HbA1C testing with a result of 42-47mmol/mol confirming IGR. Each individual with IGR is given IGR specific lifestyle literature and is supported by primary care colleagues to develop achievable aims using an individualised goal planner. Patients are recorded on the primary care IGR register and offered an annual review. A referral is made to lifestyle services which offer one-to-one individually tailored IGR lifestyle advice and facilitated access to lifestyle services. Lifestyle providers have been specifically trained in IGR with both primary care and lifestyle providers using consistent literature and advice based on detailed insight work.
Insight work undertaken as part of pathway development used the Department of Health’s Healthy Foundations Life-stage Segmentation model to develop the key messages that support people to make lifestyle changes.
A key finding was the importance of language when discussing IGR. A number of terms for IGR were tested including ‘pre-diabetes’, ‘high risk’ and ‘non-diabetic hypo-glycaemia’. People who had risk factors for IGR selected the term ‘borderline diabetes’ as it was felt they could do something to prevent or delay the onset of Type 2 diabetes.
The term ‘borderline diabetes’ has been a challenge for many professionals who did not recognise this as valid however as the insight demonstrated that ‘borderline diabetes’ was the most effective term to communicate IGR and motivate for lifestyle change, the decision was made that this would be the primary term to use throughout the patient literature.