This project aimed to reduce the number of hypothermic babies admitted to a tertiary neonatal unit by developing improvement interventions.
Our benchmark was for 90% of babies to have an admission temperature within the normal range (as per our local hospital guideline, 36.5-37.5°C).
BACKGROUND
Thermoregulation is a critical aspect of newborn care. The close association of hypothermia with increased morbidity and mortality has been well documented.
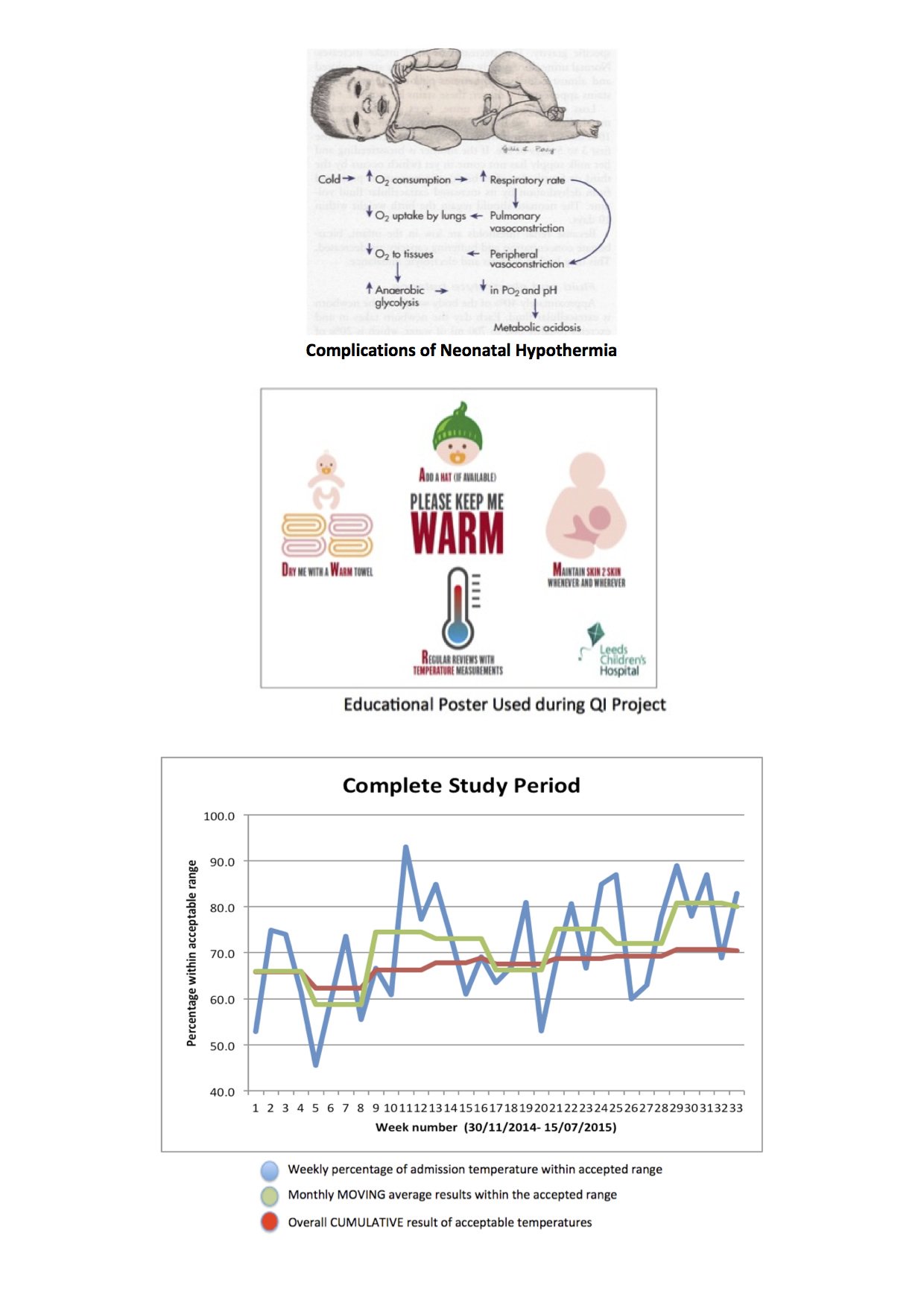
Consequences include hypothermia, respiratory distress and metabolic acidosis. A local audit revealed hypothermia was present in 23% patients on admission.
The majority of these were small-for-gestation term babies. Causes included prolonged delivery/resuscitation, deviation from thermoregulation guidelines and delay in checking initial temperature. A working group was developed to instigate changes in practice.
METHODS
The project was conducted from November 2014 to June 2015 in Leeds Teaching Hospitals Trust. PDSA (Plan-Do-Study-Act) methodology was followed.
It was co-ordinated by the consultant lead and included members of the multi-disciplinary team (doctors, neonatal nurses, midwives).
All gestational ages were targeted. Axillary thermometers were used to take admission temperature and BadgerNet was utilised to capture this.
Pre-intervention information was collected over a 3 month period.
Changes were subsequently implemented on a monthly basis; producing educational posters, addressing skin-to-skin practice, use of hats and measuring temperature before transfer.
Educational posters were placed in each delivery room and by the resuscitaire in theatre. They aimed to prompt staff about the importance of skin-to-skin and drying babies with a warm towel.
Skin-to-skin guidance was updated to support this and training given to maternity staff. Use of hats were encouraged for both preterm and term babies. Temperatures were recorded on delivery suite before transfer to the neonatal unit. This permitted an opportunity to immediately address any temperatures outside the normal range. Several midwives were identified as champions for the project. Exclusion criteria included babies undergoing cooling, outborn babies and admissions from the postnatal ward. Results were regularly updated and run charts disseminated throughout the department.
RESULTS
Pre-intervention analysis showed a cumulative baseline of 65.9% with acceptable admission temperature (see chart).
Each subsequent intervention raised the cumulative percentage further.
The cumulative average by week 33 was 70.7%.
Checking the temperature prior to transfer had the greatest single impact with 80% admissions within range for that monthly period.
Despite the overall upward trend there was still inter-variability between individual temperatures.
The lowest admission temperature was 34.2°C. The highest was 40°C.
CONCLUSION
This project has significantly reduced the number of hypothermic babies admitted to the neonatal unit.
Subsequently, associated complications have decreased.
The local unit is now exceeding national averages.
Recording temperature 15 minutes after birth had the most significant effect.
Large variation still exists on an individual level.
Further improvement is paramount in order to meet our target range.
This project facilitated understanding of PDSA methodology and the value of quality improvement in the workplace.
Lessons learnt included the importance of reiterating information, use of motivated champions and regular feedback to highlight success.
The main barrier to improvement was changing established practices/attitudes.