Time taken for the stages of the discharge process
We used a review of patient complaints relating to medicines at Lancashire Teaching Hospitals to drive improvement in TTO processes. We identified that a high proportion of complaints related to poor experience at the point of discharge from the hospital, largely due to delays in receiving discharge medicines.A review of incident reports regarding patient safety issues at discharge also identified aspects of the process in need of improvement. Having recognised the issues arising from an ineffective discharge process, the Pharmacy Department at Lancashire Teaching Hospitals undertook a project to improve the TTO process to benefit from the patients point of view as well as improving it for the Trust.
The discharge process was improved in three stages – firstly by collecting baseline data, secondly by using an Independent Prescribing Pharmacist (IPP) to write TTOs and thirdly by the introduction of a satellite pharmacy near the medical wards.
Phase 1 – Baseline data collection – Process time 8 hours and 34 minutes. A comprehensive baseline data collection was undertaken to understand the discharge process. Every step was timed so that any inefficiency could be identified, reviewed and improved without compromising safety. The data points reflected the whole TTO process pathway from the patients perspective (not just the pharmacy aspects) from decision to discharge to the medication being available on the ward. The prescribing error rate by the doctor and the accuracy of the documentation of changed or discontinued medications were also recorded. The impact of a pharmacist prescriber and a satellite pharmacy were subsequently measured using the same data collection tool.
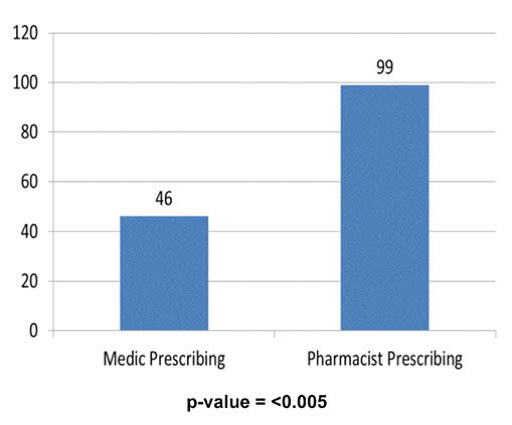
Phase 2 – Introduction of Generalist Independent Prescribing Pharmacist (IPP) – Process time reduced to just over 5 hours. Rather than using pharmacists with a niche interest - generalist IPPs were introduced to three acute medical wards (medical assessment unit (MAU), respiratory ward and gastroenterology ward). The use of IPPs reduced the discharge process to 5 hours with the decrease coming from a reduction in awaiting the TTO writing. The prescribing error rate fell from 22% to 0.7% with an IPP. The accuracy of information transferred to GPs increased from 46% to 99% with an IPP.
Phase 3 – Introduction of Satellite Pharmacy near medical wards – Process time reduced to just over 3 hours due to a reduction in TTO dispensing time. Satellite pharmacies mean that the principles of a separate work stream for urgent work and near patient dispensing can be realised. This further reduction was mainly in dispensing and transport time.
Key Outcomes
• Earlier discharge - Enhancing the patient experience, patient flow and ED 4 hour standard. Before the introduction of IPP and satellite pharmacy 14% patients were discharge before 1.30pm and this has now increased to 50%.
• Reduction in the prescribing error rate - 22% when medics were prescribing compared to 0.7% when IPPs were prescribing.

• Improved transfer of accurate information to primary care – accuracy rate of 46% (medics) compared to 99% (IPPs).

Additional benefits realised from introducing the new process for discharge:
• Medical staff time released for other patient care activities.
• Enhanced pharmacy relationships with the multidisciplinary team.
• Recruitment and retention of pharmacy staff.
The team of prescribing pharmacists at Lancashire Teaching Hospital has since been expanded to provide the services outlined above to all acute medical wards. Plans are in place to train more prescribing pharmacists and expand the team further so that the model can be implemented Trust-wide across all clinical specialities.
The trust has produced a brief video, you can see it here - https://www.youtube.com/watch?v=jFKeWPADmBQ
Further information can be found in Journal of Medicines Optimisation Volume 2 Issue 1 March 2016 available at www.pharman.co.uk