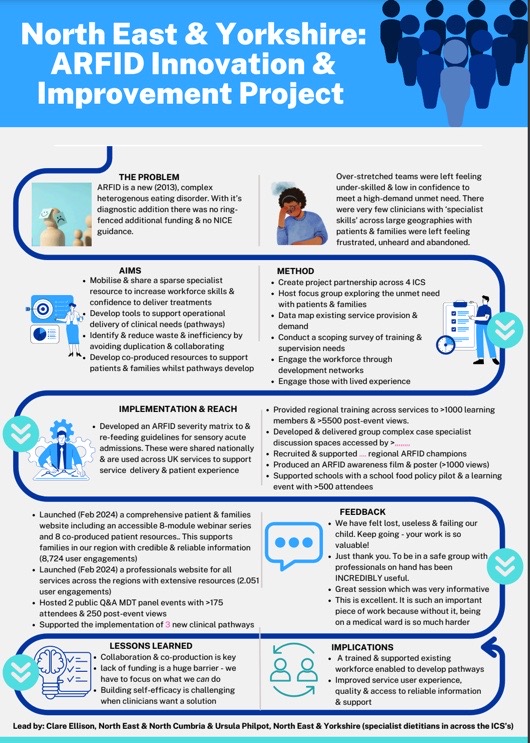
The Problem
ARFID is a new (2013), complex heterogenous eating disorder. With it’s diagnostic addition there was no ringfenced additional funding & no NICE guidance. Over-stretched teams were left feeling under-skilled & low in confidence to meet a high-demand unmet need. There were very few clinicians with ‘specialist skills’ across large geographies with patients & families were left feeling frustrated, unheard and abandoned.
Aims
- Mobilise & share a sparse specialist resource to increase workforce skills & confidence to deliver treatments.
- Develop tools to support operational delivery of clinical needs (pathways)
- Identify & reduce waste & inefficiency by avoiding duplication & collaborating
- Develop co-produced resources to support patients & families whilst pathways develop
Method
- Create project partnership across 4 ICS
- Host focus group exploring the unmet need with patients & families
- Data map existing service provision & demand
- Conduct a scoping survey of training & supervision needs
- Engage the workforce through development networks
- Engage those with lived experience
Implementation and Reach
- Developed an ARFID severity matrix to & re-feeding guidelines for sensory acute admissions. These were shared nationally
& are used across UK services to support service delivery & patient experience
- Provided regional training across services to >1000 learning members & >5500 post-event views.
- Developed & delivered group complex case specialist discussion spaces
- Recruited & supported regional ARFID champions
- Produced an ARFID awareness film & poster (>1000 views)
- Supported schools with a school food policy pilot & a learning event with >500 attendees
- Launched (Feb 2024) a comprehensive patient & families website including an accessible 8-module webinar series and 8 co-produced patient resources.. This supports families in our region with credible & reliable information (8,724 user engagements)
- Launched (Feb 2024) a professionals website for all services across the regions with extensive resources (2.051 user engagements)
- Hosted 2 public Q&A MDT panel events with >175 attendees & 250 post-event views
- Supported the implementation of 3 new clinical pathways
Feedback
- We have felt lost, useless & failing our child. Keep going - your work is so valuable!
Just thank you. To be in a safe group with professionals on hand has been INCREDIBLY useful.
Great session which was very informative
This is excellent. It is such an important piece of work because without it, being on a medical ward is so much harder
Lessons learned
- Collaboration & co-production is key
- Lack of funding is a huge barrier - we have to focus on what we can do
- Building self-efficacy is challenging when clinicians want to be given a solution
Implications
- A trained & supported existing workforce enabled to develop pathways
- Improved service user experience, quality & access to reliable information & support
You can read more about the work Lead by: Clare Ellison, North East & North Cumbria & Ursula Philpot, North East & Yorkshire (specialist dietitians in across the ICS’s)and download the poster