Over the last year rolling out the programme has continued with positive results benefitting our patients and staff alike. The last year has included - fully established MDT board rounds following a standardised format to ensure consistency and clarity in approach. By stating...
1) WHAT is the plan today to ensure this patient has a day of value towards discharge or preplanning toward discharge.
2) WHO is going to undertake that task? Therefore people have ownership and accountability and not assume that somebody else is doing this task.
3) WHY. Have all options been explored and procedures, tests, treatments, care packages, paperwork etc. need to be done as an inpatient.
This is then set for the day and the team meet again for about 15 mins in the afternoon to report the outcomes for tasks set for individual patients and the next steps required. This avoids repetition the following day and handovers can be updated with the most up to date progress for the oncoming teams. This process has full support from the executive team and heads of nursing. Other processes to engage teams include:
• Regular teaching on SAFER at doctor inductions
• Regular teachings at band 3,5,6 induction and leadership course of the SAFER patient flow bundle
• Social media and trust communications drive of process (including screen savers) of SAFER and Red2green
• Building networks and sharing ideas with other organisations
• A bespoke SAFER suite of metrics designed to show improvement and sustainment at ward level for all to access • Matrons attending board rounds to ensure sustainment
• SAFER processes must be undertaken as part of ward accreditation • Expansion of the discharge team to attend board rounds, so discharge planning can start at the point of admission. What has the impact been one year on?
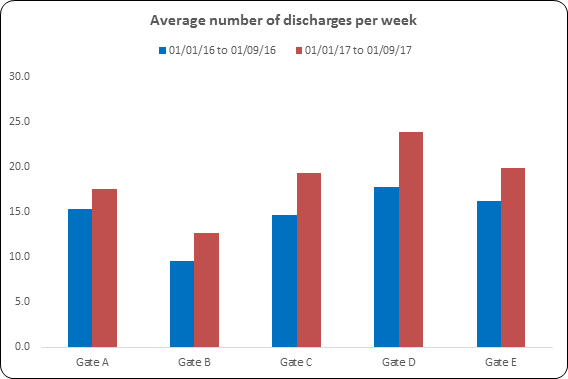
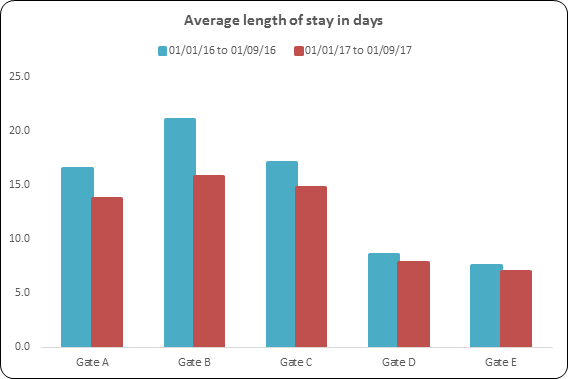
The chart below shows a visual representation of the results we achieved on four medical wards and one surgical ward, over a nine month period, compared to a nine month period before SAFER was introduced. It has helped changed the way of working at Mid Yorkshire to focus on valuing a patient’s time and reduce the amount of time needed to stay in hospital, it has also given us a greater understanding of delays and the steps we need to take to reduce these.
This process is now on 20 wards across the organisation and continues to roll out on the remaining wards.
For further information contact: [email protected] (Matron) [email protected] (Deputy Head of Nursing)
