Here is our journey over the last four weeks. We have described how we have approached implementation and the impact we have seen. We hope this helps others starting out on their journey to implement the SAFER patient flow bundle.
We worked with the Emergency Care Improvement Programme (ECIP) to introduce the ward team to the SAFER patient flow bundle and help implement it. Our approach:
- Introducing the SAFER patient flow bundle through PDSA cycles including:
- Establishing an MDT board round each day at 9am.
- Using 3 questions to focus the board round outcomes.
- Introducing the golden patient of the day, who can go to the discharge lounge by 10 am.
- Establishing EDDs (expected date of discharge).
- Assigning board round actions.
- Identification of medically fit patients.
- Establishing EDDs
- Afternoon huddles each day at 2.45 pm to mop up actions assigned at the morning board round, discharges for today, the next day and a focus on patient safety overnight.
- Training of staff and preparation for the roll out of SAFER to the next ward.
- Matrons leading length of stay reviews for stranded patients (patients with a length of stay greater than 6 days) focusing on the top 5 patients on the ward.
- Skilling up the matrons for the ward to enable them to sustain the focus of SAFER implementation on wards.
- Actions to determine the next step of the patient pathway which are allocated to a lead person.
What has the impact been?
- Length of stay appears to be reducing, at the start of the PDSA length of stay was 16 days, today it is 9 days, we will be monitoring this over a longer time period to understand the full impact.
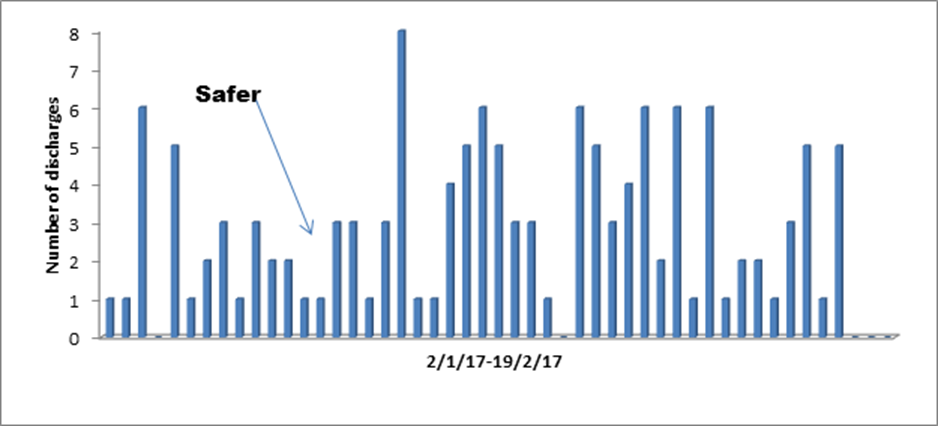
- Discharges have increased (see chart). Previously the ward averaged approximately 1-2 discharges a day and it is now 4-5 patients a day.
- Utilisation of the discharge lounge has increased. Previously 2 patients a week went to the discharge lounge, now the ward sends at least 1 patient every day.
- Weekend discharge. Previously the ward saw very few or no weekend discharges. Over the last 4 weeks there have been between 2-6 discharges at the weekend.
- Discharges by 10am and midday are increasing. Over the last few days there have been 2 empty beds by 10 am on the ward available through early discharge.
- We compared the discharges for this year with the same period last year. We have had 73 discharges during the period 16.1.17-6.2.17 compared with 45 for the same period in 2016.
- The ward stranded patient measure (patients with a length of stay greater than 6 days) for the ward before implementation was 83% compared with 61% when SAFER was implemented.
- We have had the support from our executive team who have attended some of the board rounds to celebrate our success.
- We have made the data available for the ward team so they can see the impact of the SAFER patient flow bundle.
- A run chart is completed and visible on the ward showing the number of discharges alongside safety data, so that the MDT can see the impact.
For further information contact:
[email protected]
[email protected]
[email protected]
[email protected]