The Hive would like to champion a fantastic piece of improvement work taking place in Children’s Nursing and Therapy more specifically improving the preparation/transition of young people as they move from children’s services to adults’ services.
What is the problem that needs improving?
The young patient had a heart condition, and they did not attend their outpatient's appointment once they became 18 years old and they didn’t understand the importance of taking their medication. Their mum always “sorted it”. When they were 20, they attended A&E having collapsed.
The young patient is 17 years old and has complex needs and a life limiting condition. Their mum is frightened what will happen if they are admitted to an adult ward. They have a detailed Hospital Passport and emergency care plan in place with agreed reasonable adjustments they need a carer with them in hospital.
Young people and their family too often have poor experiences like this when transitioning between children’s services and adult services and as a result they can feel unprepared for a self-care option in an adult care model. This puts their future health at risk and providers need to work differently to ensure our children become healthy adults.
Developmentally young people aged 11-19 are experiencing, physical, mental, hormonal, and social changes. Health care provision needs to improve to be more reflective of this important transitional period. Currently, young people with long term health conditions are in danger of not engaging with services because they do not understand, leading to poor management of their lifelong conditions. This may result in them presenting to health services as adults in crises.
In a new UHMBT Transition Coordinator role, Val Baxter is leading on initiatives to make transition seamless. Making sure young people are equipped with knowledge, skills, and confidence to manage their long-term condition. And for those young people, who because of mental capacity, will be unable to provide self-care, robust transition planning is required to support parents/Carers as well as the young person.
What does success look like?
Ultimately, there needs to be an improved and more age-appropriate communication between young people and services. Services that adapt to young people’s views and needs, that are ultimately central to the service design. This means:
- Trust wide understanding of developmentally age-appropriate care.
- Youth Engagement – like the relaunch of Youth Forum
- Children’s services understanding adult models of care e.g., episodes of care and patient-initiated follow-ups.
- Closer working with the community, primary care and third sector to address wider determinants of health.
- Digitally shared patient held record and development of technology.
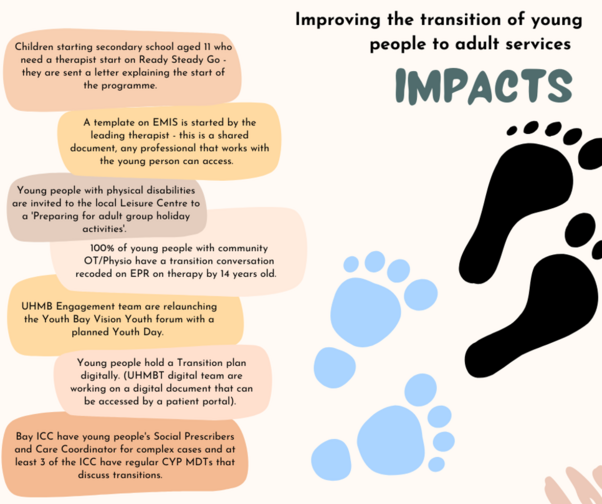
As you can probably tell, this is a large-scale piece of work, and it will be some time before we see the desired outcome. With the support of improvement tools such as driver diagrams and PDSA cycles, there are a series of change ideas being identified and tested. This Includes the engagement of a huge number of stakeholders. Young people with complex needs often have large numbers of professionals involved. For example, in one case study there was 56 different professionals involved in the care of one young person.
Change idea – Ready Steady Go
One such change idea is the implementation of the ‘Ready Steady Go’ framework.
Ready Steady Go is a set of tools developed by Southampton Hospital that helps the communication between the young person and health professional throughout their adolescent years, helping them to feel more confident and empowered and happier when they leave the paediatric service.
Watch this video to find out more about Ready Steady Go!
Some of the changes that are underway in the Women and Children’s Care Group
What does improvement look like? – Diabetes
There are already good examples of successful transition. For example, our Diabetes service who:
- Encourage their patients from an early age to take on management of health using ‘Goals for Education’ documentation on EPR.
- At 14, patients are encouraged to attend clinic sometimes on their own.
- At 16, patients have a joint clinic with a paediatric nurse and adult consultant.
- Furness General Hospital have a young person’s clinic for those 18-25 years.
- There is a 3-year process where the patient can choose to transfer anytime, when they feel ready.
What is next?
The work does not stop here. Look at some of the next steps.
- Roll out training of teams on adolescent care and Ready Steady Go and other supportive Transition Tools.
- Strengthen links between Adult and Children's Care groups – e.g., Adult Service Transition Champions.
- Patient surveys, engagement events and audits will take place to test if the improvement ideas are affecting the patient experience.
- Continue support individuals and teams with complex transitions.
- Development of joint pathways and supporting policies across the Trust.
- Auditing change ideas.
If you would like to improve the experience of your young patients and would like to link in with the work then please do not hesitate to get in touch by either emailing Val or The Hive using the following email addresses:
[email protected]
[email protected]
