I started my role as Chief Nurse Excellence in Care Junior Fellow (CNF) in June 2016 at Nottingham University Hospitals NHS Trust (NUH).
I started my role as Chief Nurse Excellence in Care Junior Fellow (CNF) in June 2016 at Nottingham University Hospitals NHS Trust (NUH).These roles were developed to encourage Band 5 nurses to develop their skills and to empower positive patient experiences.
They allow individuals to explore opportunities, evoke change, work with the wider team and uncover their own unique approach to nursing.
I work on the Oncology Day Case Unit (ODCU). The area is shared with the Specialist Receiving Unit (SRU), a busy emergency admissions area, which receives patients from specialties across the Trust. SRU has 16 beds, ODCU has 12.
Historically, when patients receiving chemotherapy treatment for cancer became unwell (including a raised temperature of 38 C or above), they were routinely admitted to SRU and given intravenous antibiotics.
I was curious to see if we could nurse these patients more effectively. Therefore as part of my CNF project, I investigated if the ODCU team could support and enhance the care of patients suspected to have neutropenic sepsis.
Over a 3-month period, I gathered data on all patients admitted to SRU who had been suspected of having neutropenic sepsis. I analysed the data to determine diagnosis, length of stay and treatment whilst in hospital. The data suggested that a substantial number of patients could avoid admission and antibiotic treatment, so I took my findings to my manager and department leaders.
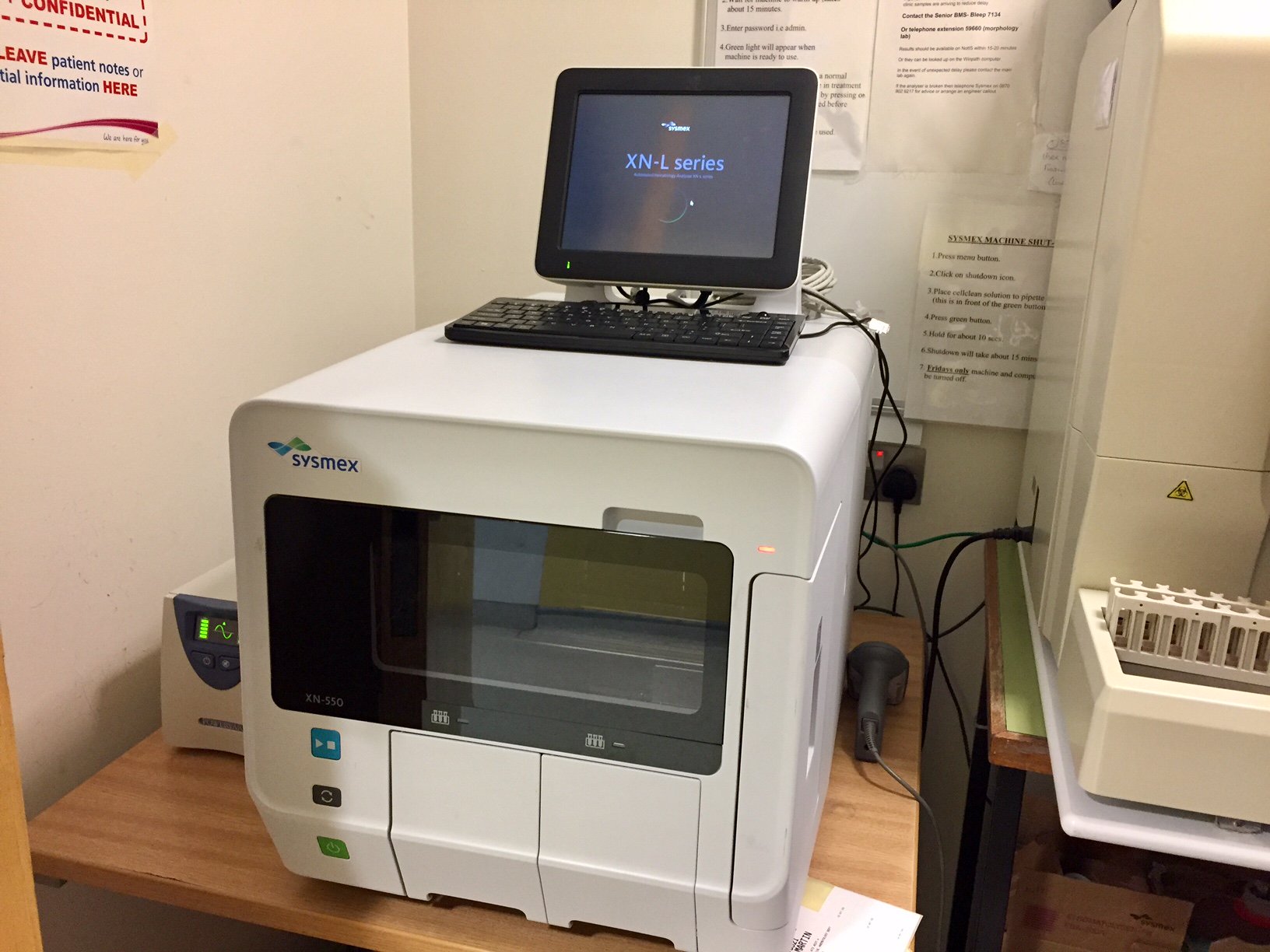
Starting in November 2016, we trialled the routine analysis of patients’ full blood count (FBC) levels on arrival to SRU, rather than administering intravenous antibiotics as the first treatment option.
To do so we used a blood analysis machine available with an adjacent day case area - the Haematology Day Case Unit. If sepsis was confirmed they were admitted to SRU, if they were not neutropenic they remained on the ODCU, were reviewed by the ward doctor and discharged home with required medication.
We continued to monitor patient and service data from November 2016 to February 2017.
Over this 4-month period, admissions reduced by 47% (from 73 to 34). The inappropriate administration of intravenous antibiotics reduced by 77% (from 73 to 17) and the National and Trust guidelines on meeting door to needle times hit 100%.
These results show the value of supporting front-line staff to innovate and provide solutions that maintain quality while also enhancing value and efficiency.
I too am more satisfied with the quality of nursing care we provide for patients and am excited to be taking this work forward with the support of Cancer and Associated Division colleagues.
There is further work to do to continue improving and we are closely monitoring the outcomes.
We recognise that we need our own blood analyser on ODCU and we intend to put this in place.
This is the result of a supportive team - without a good foundation and a team that embraces change and works together, any idea remains that – just an idea.
Fab stuff submitted on behalf of [email protected] - who was too humble to submit it herself....