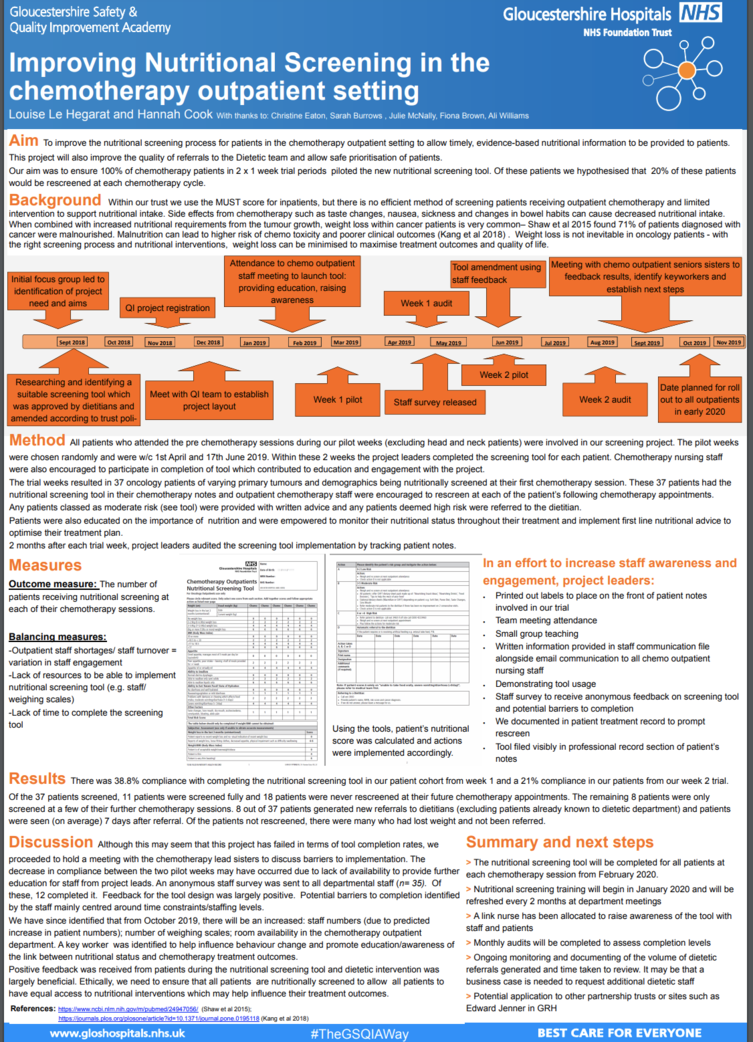
Improving Nutritional Screening in the Chemotherapy Outpatient Setting
Quality Improvement Description Background & Problem:
The current nutritional screening process in the chemotherapy outpatient setting is implemented intermittently which means patients are not provided with the appropriate nutritional intervention to aid their clinical outcomes and quality of life.
Current patient referrals tend to contain little information and tend to be when patients are really struggling. We are hoping to generate proactive referrals as opposed to reactive.
Aim:
To improve nutritional screening and increase provision of nutritional intervention for patients in line with expectations within a centre for excellence for cancer care.
100% of patients within our trial were to be screened and we aimed for 20% of these patients to be rescreened.
Method:
All patients who attended the pre chemotherapy sessions during our pilot weeks (excluding head and neck patients) were involved in our screening project. This resulted in 37 oncology patients of varying primary tumours and demographics. These 37 patients had the nutritional screening tool in their chemotherapy notes and staff were made aware of these trial patients and the need to rescreen at each of the following chemotherapy appointments.
Project leaders audited the screening tool implementation by tracking patient notes.
Results:
Of the 37 patients screened, there was 38.8% compliance with completing the nutritional screening tool in our patient cohort from week 1 and a 21% compliance in our patients from our week 2 trial.
8 out of 37 patients generated new referrals to dietitians (excluding patients already known to dietetic department). Of the patients not rescreened, there were many who had lost weight and not been referred.
Implications:
8 patients received nutritional advice and the intervention received positive feedback from patients.
After project completion and review, nutritional screening is due to be made compulsory for all patients receiving chemotherapy in CGH.
Louise-Le-Hegarat-Hannah-Cook---Poster.
Quality Improvement Presenter(s)
Louise Le Hegarat – Oncology Practice Development Nurse
Hannah Cook- General Oncology Dietitian at time of project (now Head and Neck Specialist Dietitian)
Quality Improvement Team
Christine Eaton – RGN Oncology outpatients and Nutrition link
Sarah Burrows and Julie McNally – Senior Sisters Oncology Outpatient Department
Fiona Brown – Lead Dietitian
Ali Williams- FOCUS
