Felstead is a respiratory ward and can be found in Broomfield Hospital (Mid Essex) and it is here we find ward manager Julie and Sarah (junior sister). Their ward was chosen to be part of an exemplar ward programme implementing the SAFER patient bundle ( http://fabnhsstuff.net/2015/08/26/the-safer-patient-flow-bundle/ ) and red and green days ( http://wp.me/p5H5EW-1tQ ) to help improve patient flow and experience, reduce length of stay and flush out the waiting patients experience whilst in hospital.
Board rounds were already routine practice on the ward but were undertaken in an office with the multidisciplinary team were seated. A basic board with patient details and a few columns of additional information were to hand to run through the patients on the ward with the aid of a handover sheet at the beginning of each day. Here patients were discussed and potential discharges identified and progress update was discussed. This was a process, which varied in purpose and productivity trying to add value to the patient’s journey and decide on the next steps.
The trust decided to commence an exemplar ward programme with ECIP (NHS emergency care improvement programme) support. As a member of the supporting ECIP team, I attended one such board round with a colleague to observe and in Julie’s usual bright and welcoming manner we were warmly greeted and invited to observe their board round which included patient details, how they were clinically and what was being done or waited for. There were mixed responses to the awareness of the SAFER patient flow bundle and a variable approach to red and green days, both were not being utilised to their maximum potential, missing an opportunity to identify constraints in the patient journey.
Over the coming days I visited this ward on a number of occasions, each time being met with a warm welcome and an eagerness and hunger to learn. We would have conversations about how things were going and idea’s how simple improvements could be made. It was great to see that Julie and Sarah (along with their medical colleagues) were really challenging themselves to come up with new ways of doing things and often just needed another voice to support them to make improvements.
Their first change was to move their board round out of the office and into the ward environment, this significantly reduced the time taken to undertake a board round and improved access to the medical teams. The team would now be within the ward and huddled round a board with changes happening at a rapid rate and the ward board constantly morphing into a great communication tool for all the team to use. The team thought of simple symbols to determine whether a patient had been referred (/) for therapy as an example and whether the patient had been seen and receiving ongoing (/\) support or whether they were discharged (/_\). This enabled great visualisation of what each patient was waiting for and the required actions by the multidisciplinary team to reduce delays.
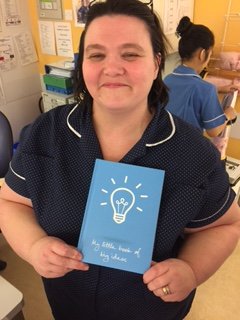
Clear EDD’s (expected dates of discharge) were used along with starting the board round with all patients deemed RED until the team could justify why the patient would have a GREEN day (a day of value). A beautiful thing to see during this time and one of the greatest achievement was the confidence and pride with which the team embraced the change and worked together to improve patient care/experience. This was especially notable within Julie, a great ward manager and leader who keeps a book of ideas for all staff members to jot down ideas as they come to them.
Early results are promising with the number of discharges improving. More than anything implementing simple rules such as the SAFER patient flow bundle and red:green days really work and help improve the urgent and emergency patient’s journey if implemented by front line clinical teams that are empowered to do so. Implementing these simple rules enables the team to flush out the constraints which can add to length of stay for patients with the potential to lead to more complex discharge requirements as a result of deconditioning. As a learned colleague always says, patients are loaned to us and it is our duty to provide the best possible experience for them, maximise their health needs and return them to their home environment. Better patient’s experience, improved outcomes and appropriate utilisation of limited resources is key to allow the NHS to provide as we would all like.