The problem:Hand Hygiene remains one of the most effective method in reducing HAIs, but the technique is largely focused on Health care workers (HCWs).
Emerging collection of evidence suggests that patient’s hand hygiene has a role in the prevention of HAI transmission including established ways to support patient hand hygiene in the healthcare settings (Knighton et. al, 2020). Involving HCWs in the process could improve compliance significantly (Sunkesula et. al, 2015). It is the aim of the Infection Prevention and control team (IPCT) to tackle rising HAI and work on systems and processes to avoid occurrence of HAI, prevent transmission and avert an outbreak.
Hospital acquired infections is key avoidable harm. Recent audit on a medical ward showed 11% compliance with hand hygiene before meals and 13% after toileting, (data from Dec 2022).
Aim
• To reduce hospital acquired infections by 50% by Dec 2023 on the pilot medical ward
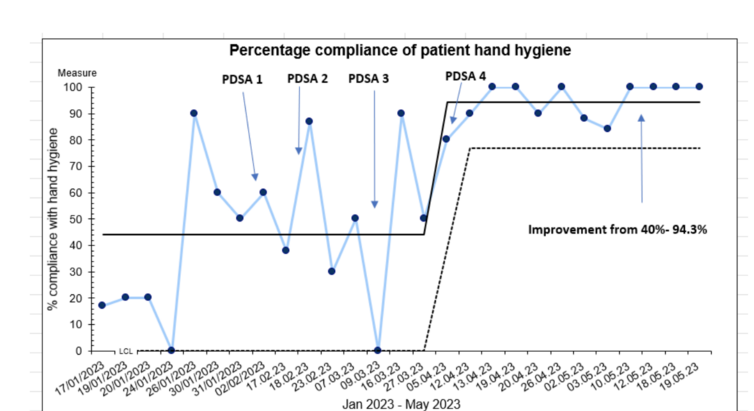
• Increase compliance of patient hand hygiene from 11% to over 60% on the pilot ward by May 2023 and over 85% by December 2023
Plan
The IPCT carried out a quality improvement project which looked into improving patient safety and quality of care by reducing risk of harm from preventable HAI by delivering a patient-centred approach through the use of a multimodal strategy to improve patient HH compliance.
- A stakeholder analysis was undertaken using the 9Cs for the quality improvement (QI) framework with the aim of identifying the key individuals who will support and empower the QI and sustain the changes (NHS Improvement 2017).
- The stakeholder with the highest interest and power created a process map and a driver diagram to demonstrate the system that is necessary to establish the necessary process to achieve the aim.
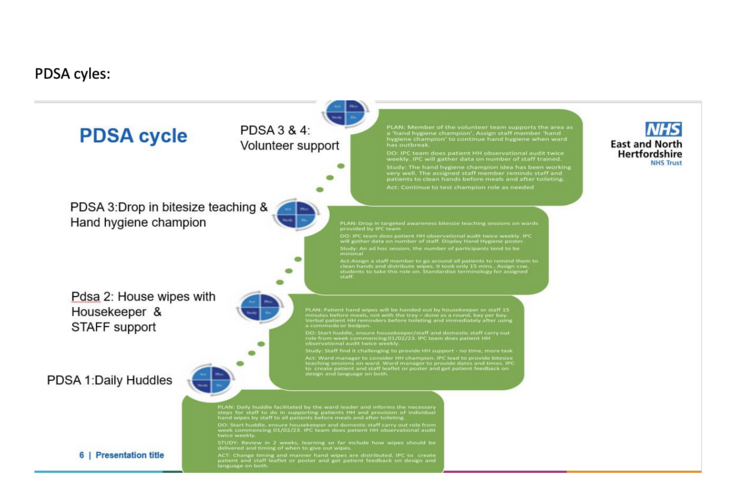
- A PDSA cycle was deployed to conduct the change ideas.
- A behaviour change wheel was utilised to ascertain interventions needed to engage and empower staff in the process to improve perspective and related behaviour in the role.
• Key drivers for change
Improve communication on patient hand hygiene
Improve hand hygiene awareness for patients and staff
Ward engagement to empower staff to support patients with hand hygiene
Patient involvement to understand how to improve hand hygiene
• The Impact:
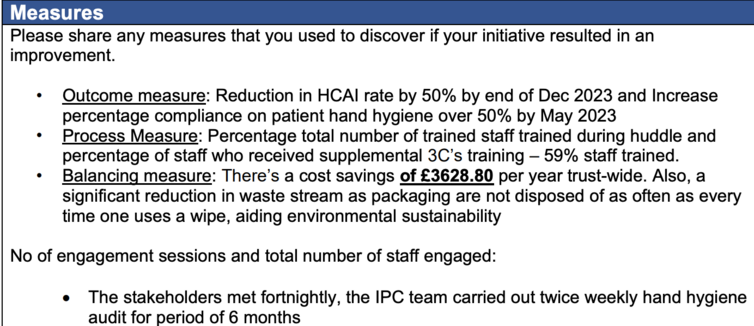
• Outcome measure: Reduction in HCAI rate by 50% by end of Dec 2023 and Increase percentage compliance on patient hand hygiene over 50% by May 2023
• Process Measure: Percentage total number of trained staff trained during huddle and percentage of staff who received supplemental 3C’s training – 59% staff trained.
• Balancing measure: There’s a cost savings of £3628.80 per year trust-wide. Also, a significant reduction in waste stream as packaging are not disposed of as often as every time one uses a wipe, aiding environmental sustainability
• Empowering staff to support improvement in patient HH using a multimodal approach has shown significant sustained Improvement
• The first aim of the improvement project was to keep HAI infections below 50% of baseline by Dec 2023. The ward managed to maintain this to between 1% to 25% for MRSA BSI, MSSA BSI, E. coli BSI, Klebsiella pneumoniae BSI, and Pseudomonas aeruginosa BSI
You can download and read the full project report HERE.pdf
See the measures in more detail HERE.pdf and the aims driver and PDSA cycles HERE
