Introduction
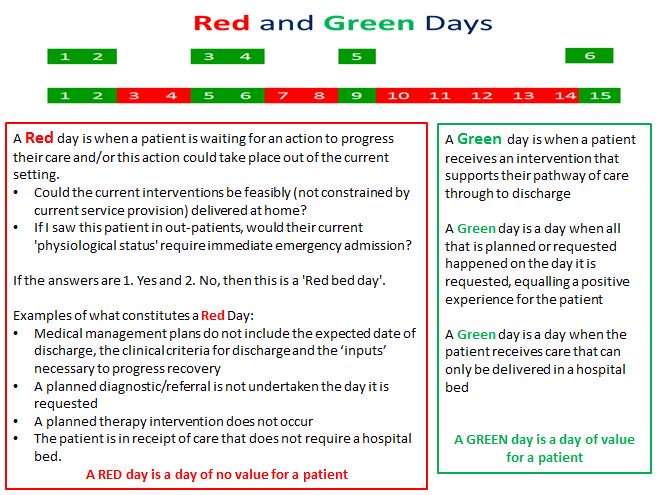
The Red:Green Bed day is a visual management system to assist in the identification of wasted time in a patients journey. It is most applicable to in-patient wards in both acute and community settings. It is not appropriate for high turnover areas such as ED, Assessment Units, Clinical Decision Units/Observation Units, and Short Stay Units where Red:Green hours/minutes may be more appropriate.
At the centre of this is the person receiving the acute care whose experience of that delivery of care is one of total involvement and personal control with expectation of what will be happening. It can be useful to consider if that person is able to answer these simple questions as soon as possible after their arrival at hospital.
- Do I know what is wrong with me or what is being excluded? This requires a competent senior assessment and discussion.
- What is going to happen now, later today and tomorrow to get me sorted out? The ‘inputs’ (diagnostic tests, therapeutic interventions etc) with specified timelines as to when things ought to happen.
- What do I need to achieve to get home? The ‘clinical criteria for discharge’, a combination of ‘physiological’ and ‘functional’ parameters. ‘Back to baseline’ is rarely a useful phrase.
- If my recovery is ideal and there is no unnecessary waiting, when should I expect to go home? This is the ‘expected date of discharge’ which should be set along with the clinical criteria for discharge at the point of admission.
A Red Bed Day is defined as a day when the patient is not in receipt of ‘care' that requires to be delivered as an in-patient, above the provision of intravenous antibiotics and usual medication and observations unless the patient is triggering on the ‘Track and Trigger’ observations. The key question is - ‘what is this patient waiting for to progress to the next phase of their care?’ It is not simply that something is happening that makes it a Green Bed Day, it is only a Green Bed Day if that process could only be undertaken as an in-patient for that particular patient’s circumstances on that day. In addition, if an investigation is being undertaken that day, the day remains a Red Bed Day until the result of the investigation is acted upon. Likewise, if a patient is due for discharge that day and the discharge prescription medications are not ready, then it is a Red Bed Day. For many patients weekends and Bank Holidays are frequently Red Bed Days. Another way of looking at this is to ask the question ‘if we saw this patient in out-patients as they are physically presenting today, would we immediately admit them to hospital?’
The rigour with which the day is judged as ‘Red’ or ‘Green’ by the teams on the Wards is the means by which unnecessary waiting can be identified and for the team to resolve that waiting. If the approach is less than rigorous, few ‘Red Days’ will be identified and opportunities for reducing patient length of stay will be lost. Those wards that are rigorous at the process will identify many ‘Red Bed Days’ and will be proactively trying to resolve the unnecessary waiting, whilst those wards that are not generating many Red Bed days or only Red Bed Days around ‘discharge processes’ are either already extremely efficient (relatively rare) or are missing an opportunity to improve care delivery and flow.
The Process
- Start the Board Round with all patients marked as ‘Red’.
- The day remains as a ‘Red Bed Day’ if there is inadequate senior presence at the Board Round
- The day remains as a ‘Red Bed Day’ if there is no clinically owned expected date of discharge (set assuming ideal recovery and no unnecessary waiting) with clinical criteria for discharge and a clear case management plan.
- The purpose of the Board round is to ensure that the patient’s case management plan is being progressed necessarily as an in-patient thus converting the day to Green. So, if a patient requires an investigation that day to progress their care, then the day will only become Green if the investigation occurs that day and there is a clear plan of what the action with regard to the result will be. Likewise if the patient has not met their ‘clinical criteria for discharge’ as yet and are receiving active interventions to get them to that state by tomorrow, the day is only a ‘Green Bed Day’ if the discharge prescription medications are ready by the evening before the expected date of discharge.
- The team assure themselves that they are clear what actions must be delivered to ensure the day is a ‘Green Bed Day’, having observations undertaken, oral medications, IV antibiotics of themselves do not make a day a Green Bed Day as these can be delivered out of hospital unless the patient is physiologically unstable.
- The Red:Green process is linked to the SAFER patient flow bundle (see below).
- The key is to link flow, safety and reliability with visual demonstration using a ‘Ward Improvement Board’ as described in the Productive Ward Programme. Ward level metrics for SAFER and Red:Green Bed Days are:
- Impact – run chart (SPC) of weekly average length of stay of discharges from the ward. The aim is for this to significantly reduce as Red Bed Days are proactively reduced.
- Process – e.g. % discharge drugs ordered and prepared the day before discharge, % of patient records with an EDD and CCD recorded in the medical notes etc.
- Balancing – number of unplanned re-admissions.
- Quality – pressure sores, HCAI, catheter days, cannula days, falls.
- The constraints identified by Wards to convert a Red Bed Day to Green need to be proactively managed by the Ward at the Board round, those that they cannot resolve need an in-day escalation process to be managed.
- The escalation process then needs to pro-actively manage the constraint. This is crucial, failure to resolve constraints proactively and just ‘reporting them’ is a ‘non value added’ reporting process.
- Link the generation of the Red:Green Bed Days to the day to day operational management strategy by standardising the ‘Operational Meetings’ using a bundle such as ‘RESPONSE’ (see below) . The escalation process can be intricately linked to the daily ‘Operational Meetings’.
- At the end of each week, the top 5 constraints that cannot be resolved by ward teams and the escalation process ought to be the focus of the system improvement programme moving forward.
The SAFER patient flow bundle (http://wp.me/p5H5EW-GM):

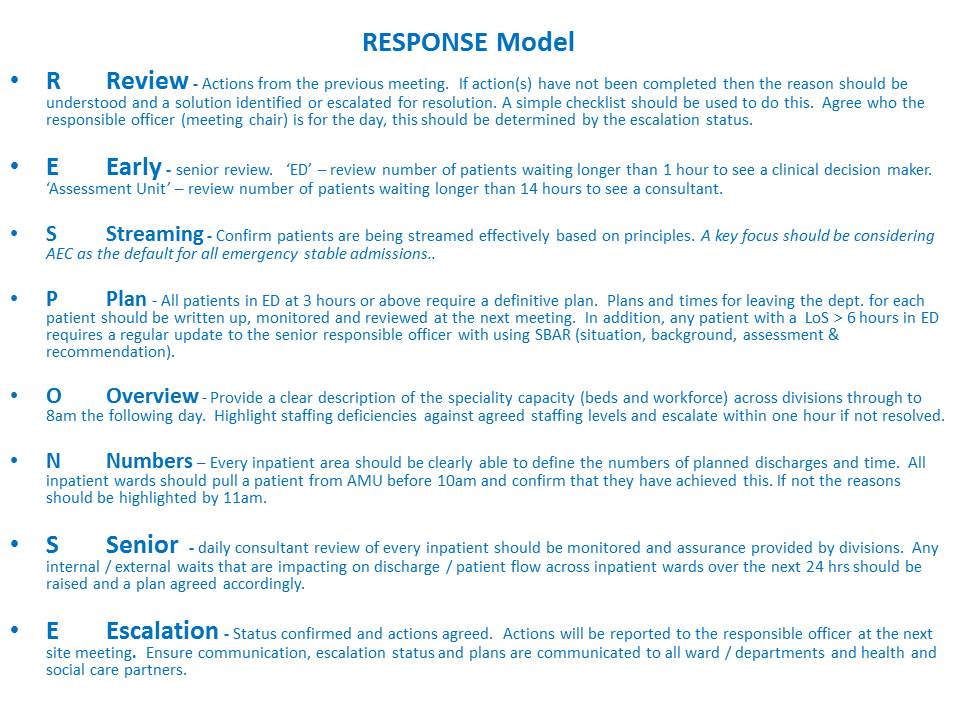
The RESPONSE Model (http://wp.me/p5H5EW-1jR):