Hospital inpatients often experience poor appetite and reduced food and fluid intake. Frail older people are particularly at risk and account for large proportions of inpatient populations. This is well recognised and measures supporting good nutrition and hydration in hospital are widely promoted.
HEFT’s innovative, effective systems and robust monitoring of nutrition and hydration were recognised in 2011, BAPEN Nutricia Good Practice Gold Award.
Adding in mobility …
It is becoming recognised that physical activity levels are also minimal in hospital, with significant clinical impact, especially in frail older people.
Keeping patients mobilising safely reduces risks, with significant benefits to clinical outcome, length of stay and cost of care, ‘deconditioning syndrome’ #endPJparalysis.
There are natural links between measures to increase mobility and those promoting good nutrition and hydration, supporting a wider focus on maintaining functional capacity in hospital, advocated by therapy teams.
At HEFT, Therapy staff (physiotherapy, occupational therapy, dietetics, speech therapy, therapy support workers) working in close collaboration with nursing teams developed a simple ‘mobility bundle’, aligned to well established initiatives promoting good nutrition and hydration.
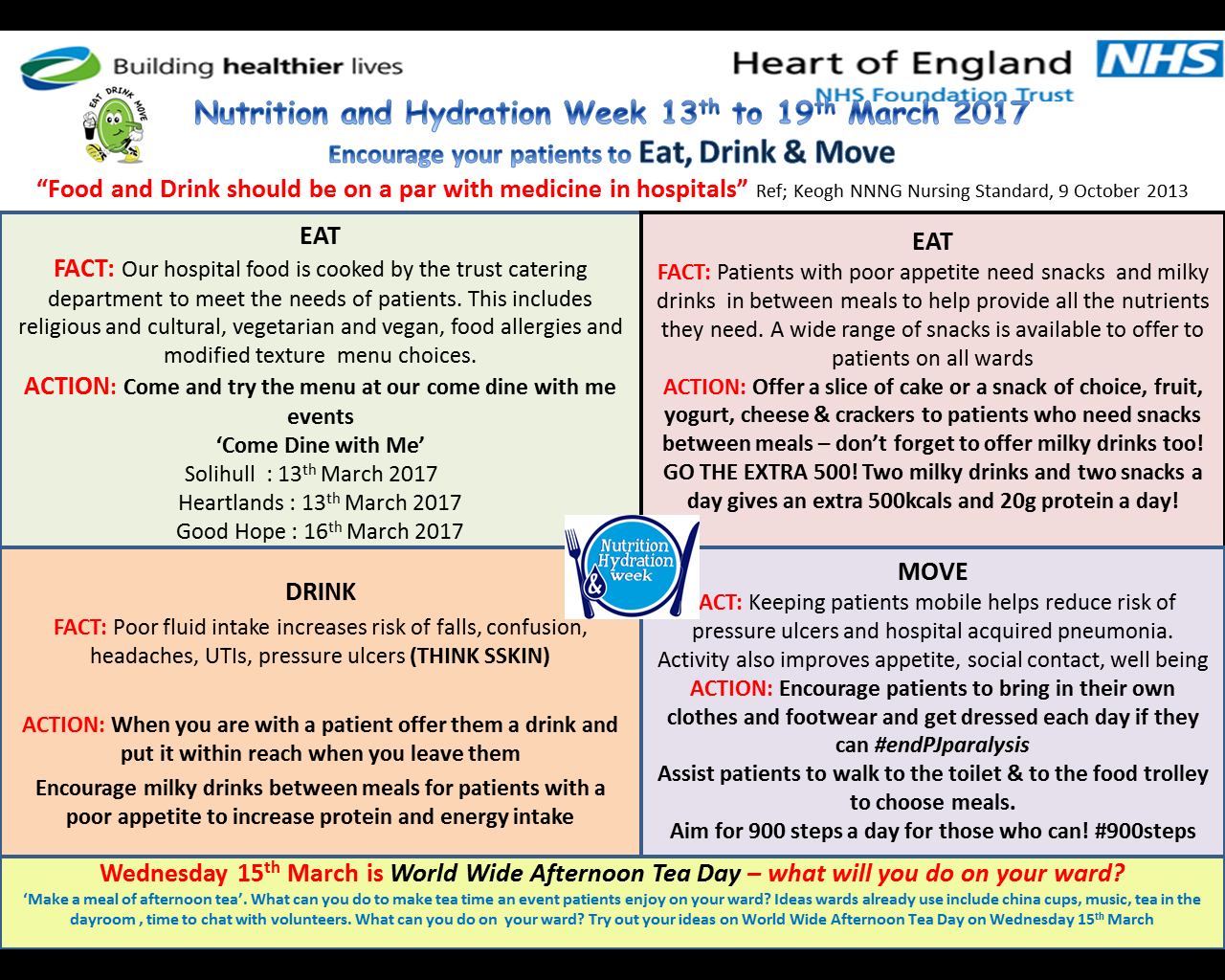
‘Eat Drink Move!’ supports health, well-being and recovery and aims to maintain functional capacity as far as possible during acute hospital admissions.
The approach also promotes benefits of keeping nourished, hydrated and mobile for longterm health.
A trial at HEFT in 2013 demonstrated the ‘mobility bundle’ was effective in increasing mobilisation and in our study reduced incidence of hospital acquired pneumonia on intervention wards by 50%.
The trial implemented the ‘mobility bundle’ on 2 medical wards (n=678 patients), comparing activity and outcomes with 2 matched wards (n=501 patients).
Patients on intervention wards showed:
increased activity (Intervention: 83.1(44.9) minutes/day, 1103(103.8) steps count/day. Control: 40.5(26.8) minutes/day, 388(90.5) steps count/day)
halved incidence of hospital acquired pneumonia (p<0.0001)
and were more likely to have a length of stay in the shortest quartile.
This relatively limited increase in activity was also recently highlighted as preventing functional decline in older hospitalised patients #900steps.
Roll out and training, critical success factors:
• Demonstrating clinical benefit of increased mobilisation secured good engagement for roll out
• Aligning to other successful initiatives: Linking the mobility bundle with measures to promote nutrition and hydration, as ‘Eat, Drink, Move!’ capitalised on good staff engagement and robust monitoring systems already supporting well embedded aspects of care
• Collaborative working between therapy, nursing and catering teams
• Taking training to ward level: Therapy teams train and promote ‘Eat, Drink, Move!’ ‘on the job’ not depending on releasing staff. The focus is on raising awareness; increasing skills and confidence to increase mobilisation; and on promoting good nutrition and hydration.
• Aligning to Trust priorities: falls, tissue viability, length of stay, admission avoidance; and national promotions Nutrition and Hydration week @NHWeek, Falls Prevention week, National Older People’s Day, #OTWeek, #DietitiansWeek.
• Building in robust monitoring to secure compliance and sustained high profile
• ‘Eat, Drink, Move!’ is highly applicable in nursing and residential care and is being shared with our community units. HEFT EDM resources: http://therapies.heartofengland.nhs.uk/eat-drink-move/