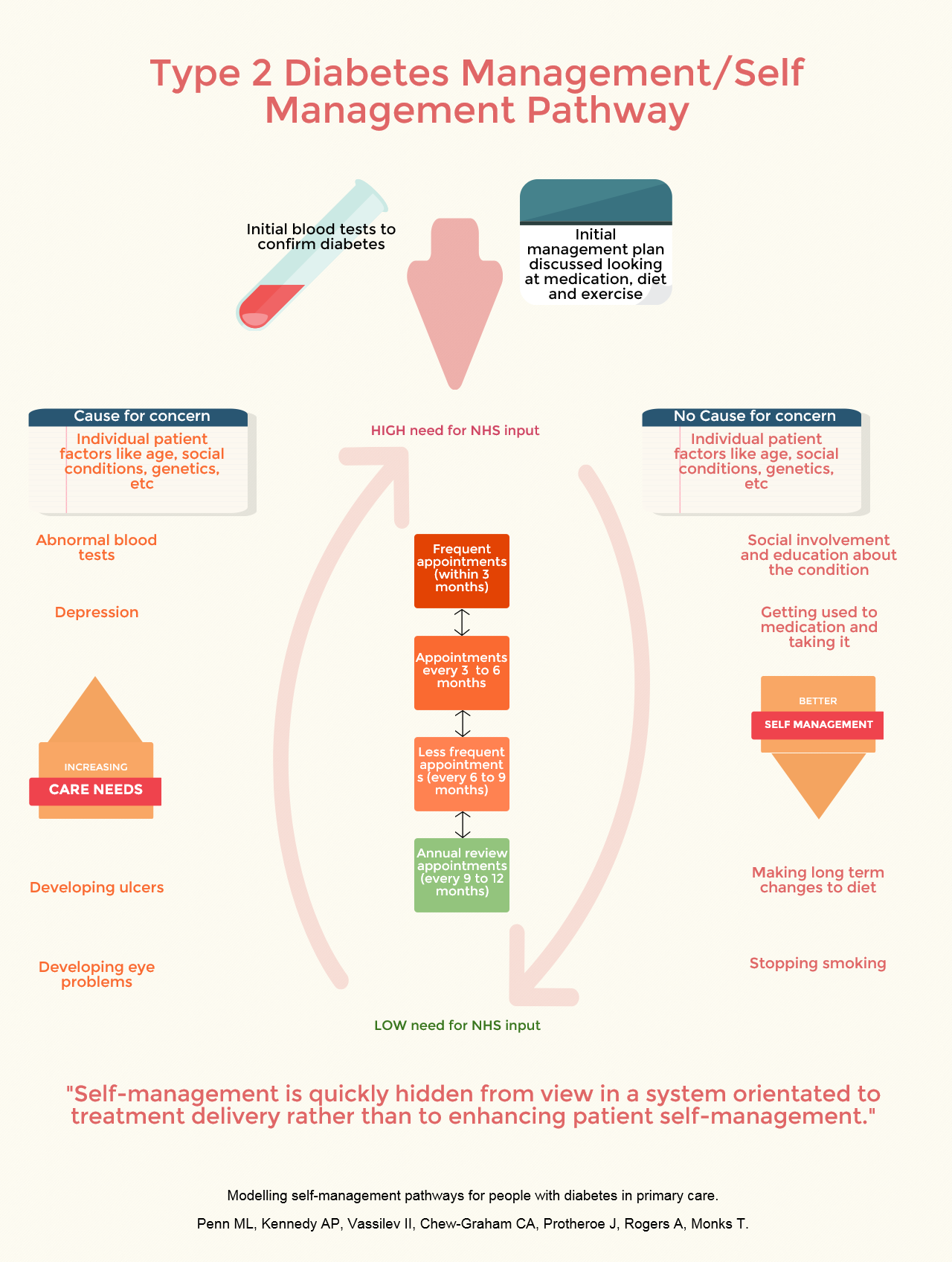
We used maps created by general practice staff to show how their patients progress through the system following diagnosis. In the current system, once treatment has been decided on, the frequency of appointments decreases and people are expected to self-manage with support from regular review appointments.
Seeing the model and talking it through with GPs and others helped us to consider some of the shortfalls in the system. The current system is very good at biomedical monitoring but this is not the same as providing support to help people manage their diabetes from day-to-day and enable a happy and active life.
Support for diabetes management needs to be a life-long consideration and people need re-assessments of the support they need to maintain healthy lifestyles. Marion Penn is a Research Fellow in Operational Research, and worked on the study: "The trial data looked at the flow of patients through services in individual GP practices, our new model brings together information from that data along with information, including patient comments, from NHS choices. It explicitly shows the connection between self-management and the need for NHS treatment, including consideration of the factors that enable or limit a patient’s ability to self-manage. It raises the questions, does the frequency of appointments actually reduce to reflect that patients’ ability to self-manage or does it follow a pre-set timetable? Are patients getting all of the support they need to self-manage effectively?" Our next phase of research will be to model systems of support outside the health service and look at how and when people use local resources, groups and organisations to help them live more healthily.
Ref: Penn M, Kennedy A, Vassilev I, Chew-Graham C, Protheroe J, Rogers A, Monks T: Modelling self-management pathways for people with diabetes in primary care. BMC Family Practice 2015, 16(1):112.