The conclusion from the study was "Conventional discharge targets like '80% by 11 a.m.' and others that spread targets across the day to balance staff workload freed up the equivalent of nine available beds for incoming patient flow, significantly reducing time spent waiting for an inpatient bed, hospital LOS and occupancy. While different strategies and workload distributions may suit individual hospital services, the study makes a strong case for improving 'early in the day' discharge timeliness to deliver better ED flow" © 2016 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine.
Most people agree that patients and their loved ones should be actively engaged in the discharge process as this promotes realistic expectations and can improve outcomes, self-care ability and patient experience.
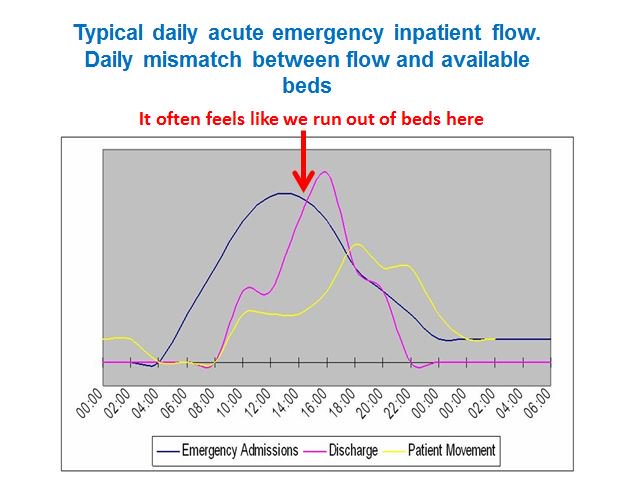
It is essential that a hospital’s discharge profile mirrors its decision-to-admit profile so that beds are available as admission decisions are made. In many cases, changing the discharge profile, so that all patients leave two or three hours earlier each day, will be sufficient to make a noticeable impact.
We often see the bulk of discharges occurring between 4pm- 6pm. The graphic below shows the effect of this - patients waiting for beds, resulting in crowded emergency departments and the late movement of patients from assessment units often with reactive management and a fire fighting approach. For patients this often means being transferred to wards (often the wrong wards) late into the evening or early hours of the morning which is unsatisfactory on all fronts.
So, what can be done to alleviate the problems of late discharges:
- One stop ward rounds - these involve most tasks that have been identified as necessary (e.g. the writing up of TTOs or the ordering of a scan) being completed before the round moves onto the next patient (or before the round starts). This avoids the batching of tasks and consequent delays. It can be useful to use a computer on wheels as an enabler. Team working is essential - leaving all the tasks to the most junior doctors is not team work
- Effective use of expected date of discharge (EDD) - The progress of every patient towards their EDD should be assessed every day at a board or ward round led by a senior clinical decision maker. Patients and / or their loved ones should be able to answer these questions:
- What is going to happen to me today?
- What is going to happen to me tomorrow?
- How well do I need to be before I can go home?
- When can I expect to go home?
Fully informed patients (and their loved ones) will be in a much better position to make arrangements for discharge rather than those that find it a surprise that they are leaving on the day of discharge.
- Transport - ensure arrangements are in place before hand. Rather than asking patients if they need hospital transport, try asking patients what arrangements they have in place. Many patients wait unnecessarily for hospital transport as they have been asked if they would like it when their family or friends would have been able to collect them. For those patients that genuinely need hospital transport ensure it is booked in advance.
- Take out drugs (TTAs/TTOs) - this is a major constraint to patients waiting on the day of discharge. These should be written up before hand or finalised during the ward round. Some trusts have made great strides to improve the TTO process (see- http://fabnhsstuff.net/2016/03/30/pharmacy-innovation-discharge/ ) which has led to patients leaving hospital earlier in the day.
- Essential equipment - if patients EDDs are set effectively and communicated with all members of the multi disciplinary team, it should be a rarity for there to be equipment delays, ordering processes should be standardised and simple.
- Carers - for those patients that require additional care upon discharge, arrangements should be made to prevent late discharge. It is inappropriate for frail older patients to arrive home late in the day.
- Use simple rules to reduce variation. The SAFER patient flow bundle is a good example of this, it's like a clinical care bundle and can help teams improve patient flow (see - http://fabnhsstuff.net/2015/08/26/the-safer-patient-flow-bundle/ ). Earlier discharge is one of the five elements of the bundle.
- Nurse led / facilitated discharge - with clear plans in notes, there is no reason why experienced nurses cannot discharge those patients. This is routine on all day surgery units (a great example of timely discharge), if it can be undertaken there, it should be possible to this elsewhere.
So, without doubt timelier discharge continues to be a consistent problem that could be significantly improved with a can do mind set, engagement of front line clinical teams and appropriate leadership
I am writing this from a hotel, I have no doubt about the date and time I will be leaving.
If your organisation has managed to improve the timeliness of discharge, why not share how you've achieved it with others and submit your story to http://fabnhsstuff.net/ecist/
