THE CASE FOR CHANGE
Consider the following statements:• Imagine leaving your home and never returning to it again
• Imagine someone tells you that you are moving house tomorrow and you have no control over where you are moving to and how much it will cost.
This is what we do to thousands of older people every year. Many older people are admitted to hospital with a mild to moderate illness on top of any pre-existing conditions. We make judgements about how the person will manage when they return home based on perceptions about the person after the effects of a stay in hospital, often prolonged. We assess them in an environment that is alien and confusing.
Some Facts:
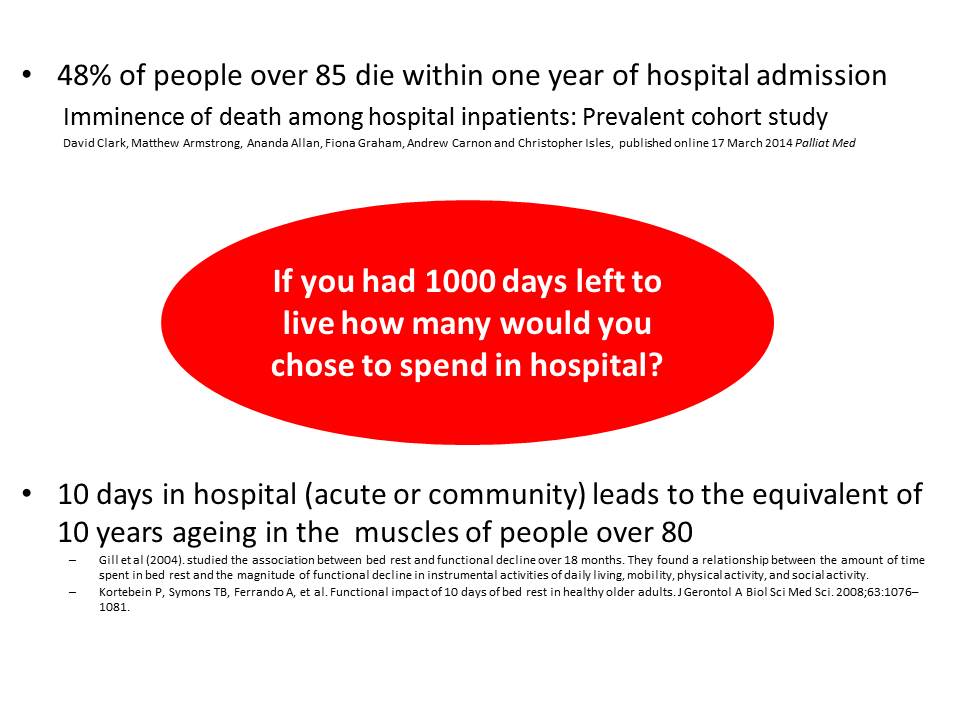
We need to ensure that people are in hospital for the shortest possible time ensuring that medical and nursing needs that can only be delivered in an acute hospital setting happen there. All lower level care, recovery, rehabilitation and re-ablement should wherever possible happen in the persons’ usual place of residence.
We currently undertake assessments of a person’s ability to live their life once they no longer require acute medical or nursing care in the acute hospital setting. This is a time consuming process, comprising a number of assessments and information gathering (described by some as interrogation) that people report feels as if they are taking an exam. It adds to the amount of time people spend in hospital physically deconditioning and is a significant percentage of the days they have left in life.
We ask people to make cups of tea in hospital Occupational Therapy kitchens, walk upstairs even when they live in a bungalow or on one level in their house. We ask them intimate questions about how they manage their personal care and then decide whether they have passed or failed these tests. For people with dementia this is even more challenging, we decide based on their behaviour in hospital that they are not safe to be at home because they are wandering, or have challenging behaviour. They may just be trying to find home as they have forgotten they are in hospital. A person may appear incontinent overnight in hospital because they cannot get to the toilet unaided and assistance can often take a while to arrive. They may have had a catheter inserted on admission despite having no significant continence problems prior to admission. The issue of going to the toilet at night is often one of the deciding factors in the perceived need for 24 hour care.
We decide whether people have ‘rehabilitation potential’, take away the word rehabilitation and we are suggesting that as an individual they have no potential. I find it interesting that we do not as therapists consider a person with quadriplegia to have no ‘rehabilitation potential’ yet decide this to be the case for many older people who are no longer as mobile as they were. We decide they cannot possibly live the way they chose to live before admission because they have not reached their ‘baseline’ level of function. I don’t know about you but I struggle to make a cup of tea as efficiently in someone else’s kitchen so might appear less capable than I believe I am in my own environment. I am also not aware that we expect younger people to be at their baseline in order to be discharged from hospital.
In trying to do what we believe to be the best to keep people safe we have become risk averse on their behalf and paternalistic in a way that would not be acceptable if we were talking about a child. The legislation that covers children requires us to involve children in the decisions being made about them. We all live differently, we are individuals and we have a responsibility to allow people to live their lives as they want to
How often do we sit in multi-disciplinary team (MDT) meetings and make decisions as a team without the person in the room, making judgements about how people live. We may then have a family meeting and, in effect inform them of our decision, appearing to consult. I have often sat in these meetings imagining they were talking about me, I find myself thinking that I would not want them to talk about me in this way without me there to express my point of view and let them know what matters most to me.
What really matters to older people are the following to their standards not ours:
- Having choice and control over their lives
- Occupation and activity, having a purpose
- Personal care and appearance
- Food and Drink
- Accommodation (cleanliness and comfort)
- Personal safety
- Social participation/inclusion
- Dignity (in care) once you are acutely ill or dependent on care
We need to work on the principle that we should support people to return home to recover from their admission to hospital and cease to make decisions about long term care in a hospital setting.
I saw the man in the picture below earlier this week on the BBC news, he's 94 and lives on his boat in the Solent and he still regularly sails out of Portsmouth harbour, what would we say if he came into hospital after a fall or with an infection? Think home first. Liz Sargeant - Integration Health & Social Care Lead (NHS Emergency Care Improvement Programme), OBE, MSCP @lizsargeant
Liz will be writing more articles for the ECIST Network on Fabstuff including:
- What we need to change
- How we need to change who does what and what we do


