Community Based Unscheduled Care Coordination - Preventing unnecessary hospital attendance and admission for sub-acute patients requiring unscheduled care.
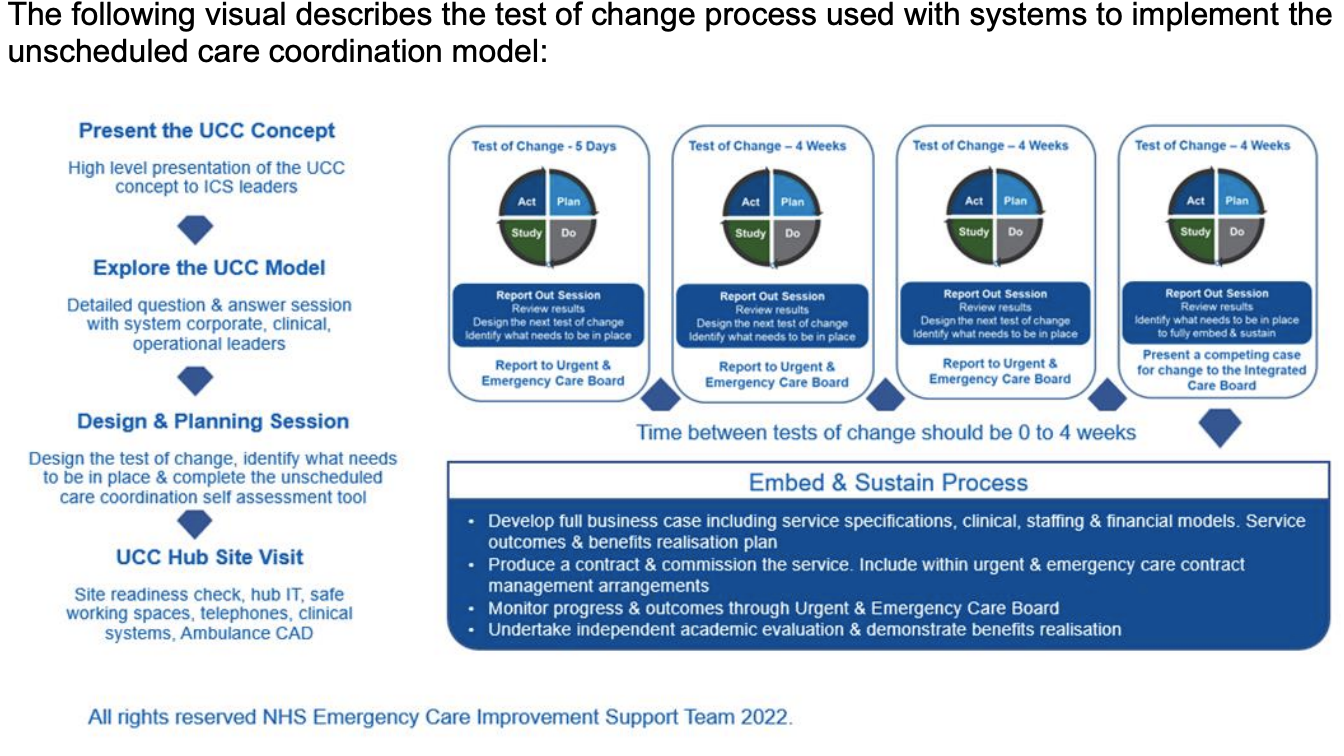
There are very few services available in real time to help community-based clinicians access the most appropriate part of the health and care system whilst they are with their patient. As a result, this leads to them working in a clinical silo, with a proportion of their patients attending hospital unnecessarily.
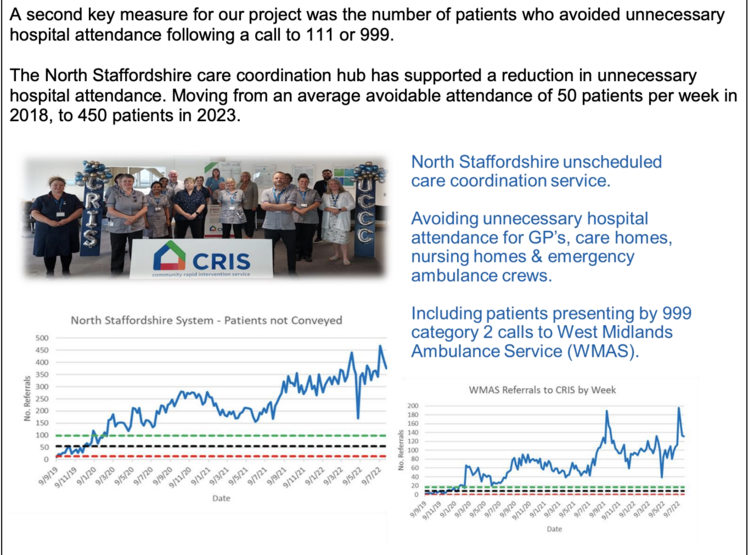
Our project tells the story of how we help systems to ensure that patients who are not seriously ill or injured, receive their care in their normal place of residence.
Plan
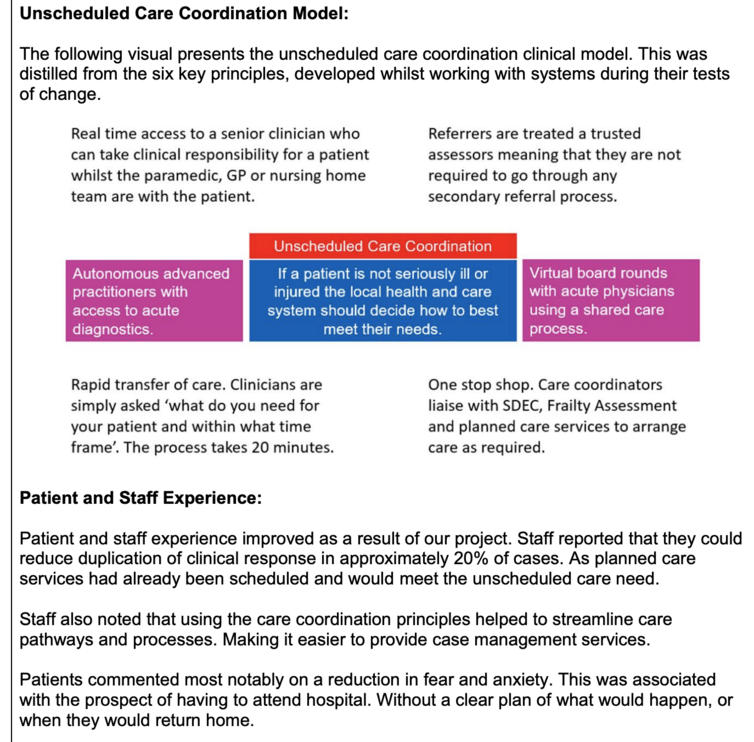
We worked with health systems to provide access to unscheduled care coordinators via a ‘genuine single point’ of access, that provides the means to respond rapidly and appropriately. Advanced clinical practitioners based in care coordination hubs take clinical responsibility at the point of call. They arrange for multidisciplinary teams to respond,providing care by default, in the patients’ home unless clinically indicated otherwise.
Systems set up care coordination hubs, to sit above all unscheduled care services. These are not a replacement or duplication of planned care access points such, as community neighbourhood teams. They operate at ICS or County level providing a ‘catch all’ service for referring clinicians.
We helped systems to develop and operate a clinical exclusion criterion, as opposed to an inclusion criterion. The was designed to accept any patient with an unscheduled care need if they are over 18 years of age, not pregnant and not seriously ill or injured. Basically, any patient without a clinical ‘red flag’.
We introduced trusted assessor status for Paramedics, GPs, community-based clinicians, and nursing home staff. Meaning that they are not subjected to further assessment and triage processes. Once the clinician has assessed their patient, the care coordinator simply asks them ‘what do they think their patient needs clinically and within what timeframe’. The care
coordinator discusses the case with the referring clinician, and they jointly decide if the patients’ needs can be met by community services. The assessment and transfer of care process takes fifteen minutes, with a single phone call. Meaning that it is a viable operational alternative for GP’s and Ambulance Crews.
Tests of change led by NHS England’s Emergency Care Improvement Support Team (ECIST) have shown, that talking to ambulance crews on scene and offering care at the patients’ home can reduce conveyance. Between 30% and 50% of crews intending to convey their patient to hospital, used unscheduled care coordination, following a clinical conversation with
an advanced practitioner.
Care coordination hubs provide the health and care system with the ability to respond to patients who are at ‘immediate risk’ of receiving an emergency ambulance or attending hospital unnecessarily. Even though they are not seriously ill or injured.
Colleagues working in care coordination hubs have the time to make the appropriate arrangements to treat patients at home or close to home. As a catch all service, this might involve liaising with local neighbourhood teams and arranging an aspect of planned care. The key aim is that referring clinicians make a single call to the hub and do not need to phone
multiple teams.
Care coordination hubs, linked to community based planned and un-planned services, showed that it is possible to reduce unnecessary emergency ambulance dispatches, ambulance conveyance, attendance at Emergency Departments and hospital admissions.
You can read and download the full project report HERE