Workforce Wizards Cancer Week -

People living with cancer may require support from a variety of healthcare professionals across numerous health care systems often resulting in fragmented and uncoordinated care. Integration of health services for people living with and beyond cancer is crucial to optimise both the quality and outcomes of cancer care but is often poorly implemented in practice (Rubin, 2015).

As more people are diagnosed with and live beyond cancer, there is an increasing recognition that hospital-based models of care are unsustainable. However, there is no clear agreement about what an effective model of integrated care for patients living with and beyond cancer might look like.
This innovative and exciting Health Education England (Wessex and Thames Valley) funded project, led by the Wessex Cancer Alliance, involves cancer clinical nurse specialists working four days a week with eleven GP practices in the Wessex and Thames Valley regions. The aim of this “boundary spanning” (Gilburt, 2016) nurse role is to promote integrated working between primary and secondary clinical teams.
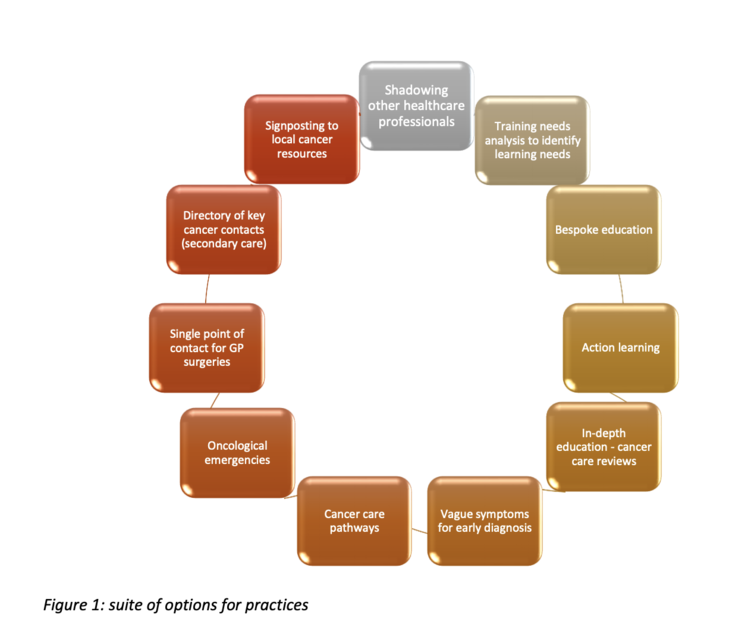
Since July 2019, primary care teams are working with the boundary spanning nurses to ensure that the new role is tailored to the needs of each individual practice. For example, in some practices, boundary spanning nurses are working directly with practice nurses to upskill them to take on cancer care reviews to complement their existing role of managing chronic disease. In other practices, boundary spanning nurses are working with other healthcare professionals (such as GPs, pharmacists or paramedics) to identify areas for training and development. Options available for practices to access are outlined in Figure 1 below:
Boundary spanning nurses are also identifying areas for reciprocal learning for specialist cancer clinicians (for example, understanding the role of primary care in providing supportive care for patients with cancer; understanding how common co-morbidities can be managed alongside cancer).
Instances of improved patient and healthcare professional experience from the project so far are:
- Hospital based clinical nurse specialists knowing whom to contact in the primary care team to discuss management of co-morbidities, reducing the workload for the patient who would have had to book an appointment with their GP surgery
- GPs able to discuss patients with clinical nurse specialists directly, resolving issues quickly rather than lengthy delays on telephone and potentially preventing an admission
For more information, please contact Kate Lippiett in the project management office [email protected]
References:
Rubin et al (2015) The expanding role of primary care in cancer control, The Lancet Oncology, Volume 16, Issue 12, pp. 1231-1272
Gilburt (2016) Supporting integration through new roles and working across boundaries, Kings Fund https://www.kingsfund.org.uk/p... [accessed 11/3/2020]
You can read the full project summary here
