Current situation: It has long been recognised in the healthcare sector that the rate of haemolysis in blood samples taken in Emergency Departments (EDs) throughout the UK, and in many other countries, is higher than in those collected in other hospital wards and departments.
There are many questions that may spring to mind:
What is haemolysis? What is the size of the problem? What can we do about it? What causes it? Why is it a problem?
What is Haemolysis?
Haemolysis: the rupture of erythrocytes, releasing the cell contents into the plasma
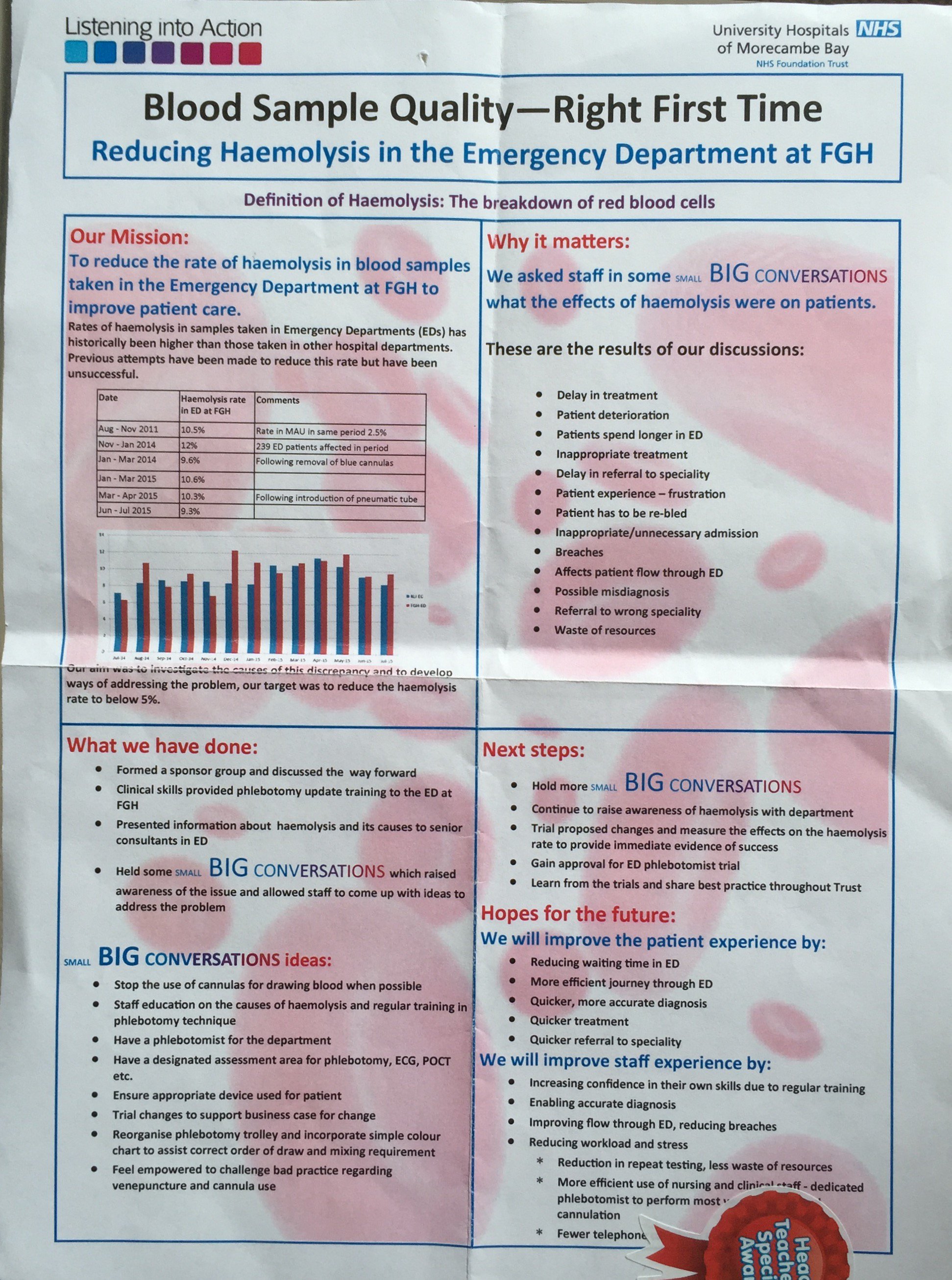
What is the size of the problem? Haemolysis rate in ED at FGH Aug - Nov 2011 10.5% Rate in MAU in same period 2.5% Nov - Jan 2014 12% 239 ED patients affected in period
Jan - Mar 2014 9.6% Following removal of blue cannulas
Following introduction of pneumatic tube Jun - Jul 2015 9.3%
•We set up a sponsor group:
ED FGH: Paul Grout, Asish Chattergee, Helen Thompson, Jo McGuire Blood Sciences: Janet Eglin, Janet Todner, Tasha Patel, Daniel Newport Phlebotomy: Carole Henderson Clinical Skills: Sharon Wall, Debbie Wagstaff LiA sponsor: John Butterworth
•Researched the issue •Discussed the problem •Provided some initial phlebotomy training •Decided on the best way to engage staff •Held SMALL BIG CONVERSATIONS with ED staff •Measured initial outcomes
SMALL BIG CONVERSATIONS
In Vitro causes of haemolysis How does venepuncture cause haemolysis?
How does haemolysis affect blood results?
Delays caused by Haemolysis
•Any physical force causing shear stress on the erythrocyte ➢Vacuum ➢Pressure ➢Turbulence ➢Small aperture
•Freezing ➢Ice crystal formation
•Cell death ➢Failure to separate cells from plasma/serum before cell breakdown
•Poor venepuncture technique –Needle not sited in vein lumen correctly –Incorrect gauge of needle chosen for vein size –Vein collapse –Too much vacuum applied by syringe plunger •Cannula use –Designed to deliver fluid, not to remove blood –Soft tube may collapse under vacuum –Drawing blood through 90o tap •Blood transfer from syringe to sample tube –Via venepuncture needle through rubber tube cap –Under pressure from syringe plunger •Excessive shaking of sample rather than gentle mixing
•Biological contamination of plasma/serum by erythrocyte intracellular contents ➢Especially Potassium (x25), LDH and AST (x40) but many others too •Analytical interference of spectrophotometric and enzymatic assays ➢Haemoglobin absorption peak at 415nm ➢Enzyme/co-enzyme interferences ➢Most mainline Biochemistry assays ➢Transfusion, as haemolysis mimics incompatibility •Analytical interference with immunoassays ➢Interference with Antibody/Antigen reactions ➢Many Biochemistry and coagulation immunoassays
•Sample collection – 5 minutes •Transport to lab – 1 minute •Clotting time, SST tube – 30 minutes •Centrifugation time – 10 minutes •Sample processing – 5 minutes •Analysis – 20 minutes •Review of results – 3 minutes •Specimen haemolysed, telephone ED – 2 minutes •Review by clinician – 5 minutes •= 81 minutes, then start again!
General discussion point: What are the effects of haemolysis on our patients?
Responses from staff :
· Delay in treatment · Patient deterioration · Patients spend longer in ED · Inappropriate treatment · Delay in referral to speciality · Patient experience – frustration · Patient has to be re-bled · Inappropriate/unnecessary admission · Breaches · Affects patient flow through ED · Possible misdiagnosis · Referral to wrong speciality · Waste of resources
Question 1: How can we reduce the rate of haemolysis in ED?
Question 2: Thinking about patient flow through ED and current protocols regarding blood collection (who/how/when/why) What changes do we need to make to achieve our aim? SMALL BIG CONVERSATIONS
Staff ideas:
•Stop the use of cannulas for drawing blood when possible •Staff education on the causes of haemolysis and regular training in phlebotomy technique •Have a phlebotomist for the department •Have a designated assessment area for phlebotomy, ECG, POCT etc. •Ensure appropriate device used for patient •Ensure most appropriate site chosen for venepuncture/cannulation Trial changes to support business case for change •Reorganise phlebotomy trolley and incorporate simple colour chart to assist correct order of draw and mixing requirement •Feel empowered to challenge bad practice regarding venepuncture and cannula use
So far we have :
•Provided some initial phlebotomy training
- Raised awareness of the causes and effect of haemolysis through presentations to the senior ED team
- •Raised staff awareness of haemolysis through presentations and discussion at SMALL BIG CONVERSATION
- •Encouraged an environment in which staff can make suggestions and think of new ways of
- Improving the patient journey, care and experience
- Improving quality
- Reducing waste
- Improving staff experience
It’s early days, as our SMALL BIG CONVERSATIONS were only held between the 15th and 29th June 2016 Next steps: •Continue to raise staff awareness of haemolysis
•Provide further phlebotomy training and competency assessment
•Trial proposed changes and measure the effects on the haemolysis rate to provide immediate evidence of success
•Gain Trust approval for ED phlebotomist trial
•Learn from the trials and share best practice throughout Trust
Hopes for the future
We will improve the patient experience by: •Reducing waiting time in ED •A more efficient journey through ED •Quicker, more accurate diagnosis •Quicker treatment •Quicker referral to speciality
We will improve staff experience by: •Increasing confidence in their own skills due to regular training •Enabling accurate diagnosis •Improving flow through ED, reducing breaches •Reducing workload and stress oReduction in repeat testing, less waste of resources oMore efficient use of nursing and clinical staff - dedicated phlebotomist to perform most venepuncture and cannulation oFewer telephone calls from Pathology
You can find the full presentation here https://www.dropbox.com/s/v364eqr6cl7tqcj/Pass%20it%20on%20Haemolysis%20presentation%20JE%20July%202016.pptx?dl=0
Reducing Haemolysis in the Emergency Department at FGH
Janet Eglin - Technical Services Manager, Biochemistry