Millions is made from services or business designed to support individuals with making life changes, coaching and supporting establishing new norms and habits in the hope that old ones don’t creep back in.
Whether making a personal change or supporting a change in patient care, it is clear that this takes time and is more complex than just changing a process or environment or simply deciding to change.
Motivation, understanding and engagement actively in the process by all involved is needed to increase the chances of success.
How are you offering the greatest opportunity for success and embedded sustained improvement within your services and bringing all involved along with you? What are your wider teams aware of? How are your communicating and providing regular updates? What involvement in what the day to day will look like have they had? Are the team moving in the same direction?
Case study: Venous Leg Ulcer Pathway (Oxford Health NHS Foundation Trust) Lessons learnt: supporting sustainable improvement outcomes
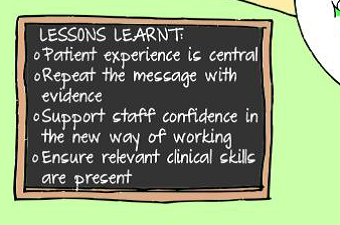
• Consider the values of those you are communicating with and adapt in accordance: Engagement from teams to adapt practice and team behaviours to the new VLUP pathway increased notably with county wide adoption when reason for the changed from being driven by commissioner reporting to prioritising priority of improved patient experience, quicker healing rates and potentially reduced demand on nursing time per presentation. A patient experience video was used.
• Repetition and consistency are essential: don’t assume that people will accept or have understood when told once, ensure a consistent message is given by all with multiple opportunities to engage staff in the message utilised.
• Use Evidence to support the message: Healing rates from the VLUP pilot team provided objective evidence and validity to the new pathway. This reduced resistance and generated increased interest and discussion with previously hesitant teams.
• Allow room for two way communication: anxiety about what new will look like is normal and will happen whether you provide space to explore it or not. Embrace this as a positive opportunity for Teams to engage in a two way exploration of the change and new ways of working. They have valuable contributions to make on what good might look like, the new VLUP PSAG was radically different when designed by clinical teams rather than management representatives and improvement team.
• Don’t assume clinical staff will feel confident with all aspects of new ways of working, support staff to build skills and confidence in new way of working
• Set clear expectations – SOPs: communicate expectations of new processes and systems clearly to support consistency and limit risk of variation
• What champions do you have to deliver the message: make use of clinicians from the pilot teams to introduce the new way of working, effective to support the message that the change is positive step in clinical care
Advised Reading: Mapping Patterns of behaviour in complex systems. Exploring the underlying factors that accelerate or impede systems transformation. Paul Plsek & Sarah Garrett (2007)