A bloodstream infection (BSI) is a recognised risk associated with parenteral nutrition (PN) administered via a central venous catheter (CVC). It can be life-threatening, leads to an extended hospital stay and, for patients reliant on PN, it can mean 7-14 days without nutrition. NICE estimate that the cost of each catheter-related BSI is £9,000.
Aim:
50% reduction in the incidence of BSI associated with a CVC in patients receiving PN in an adult ward by end of 2018.
Method:
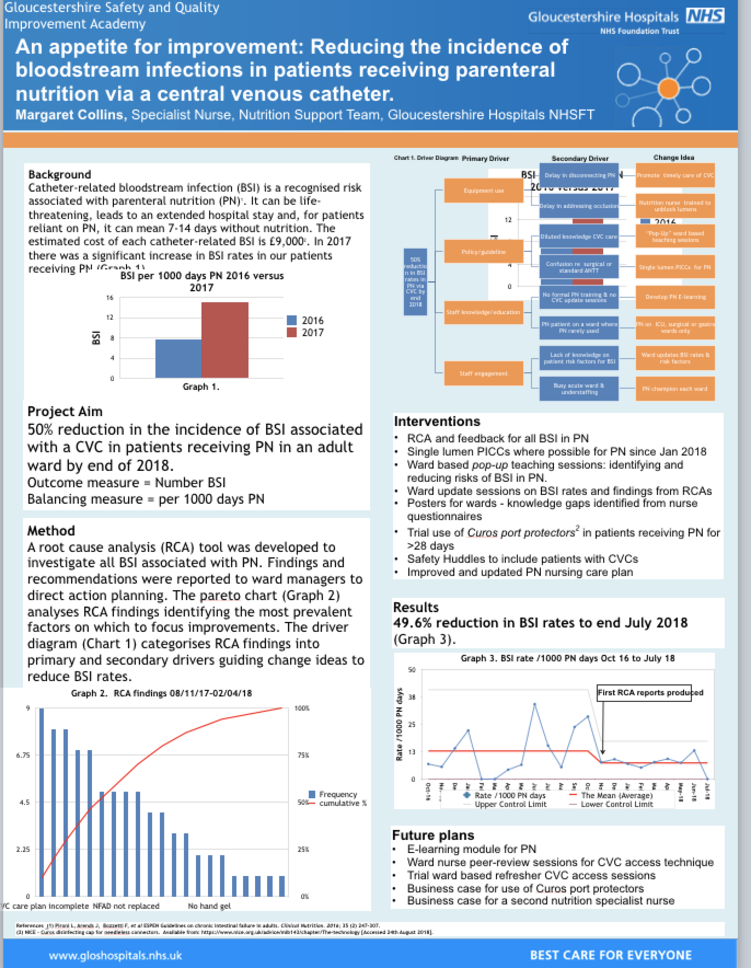
The BSI rate is recorded each month and the number of days of PN administered each month is used as a balancing measure to allow fair comparison of monthly BSI rates. Monthly infection rates were therefore recorded per 1000days of PN. The actual amount of PN administered per month was 85-216 days.
A root cause analysis tool (RCA) was developed to investigate each BSI thought to be linked to the CVC. Findings from each RCA were reported to the relevant ward manager to highlight areas which could be improved and guide action planning on the ward. Findings from the RCAs were plotted on a pereto chart to identify the most frequently occurring factors where improvement should be focused.
A driver diagram was used to plan the improvement process and identify change ideas. Engaging ward nurses, improving their knowledge and understanding of risk factors for developing a BSI and promoting best practice in management of CVCs were key aspects of this project.
Pop-up ward based teaching sessions for nursing staff were used to highlight the risk factors for developing a BSI and clarify best practice for management of CVC and PN.
We worked with the Vascular Access team to switch to single, rather than dual, lumen peripherally inserted central catheters (PICCs) to reduce the number of times the PICC was accessed.
In a small number of patients who required PN for more than 28 days, we trailed the use of a protective cleaning cap on the CVC.
Results:
We have made a 49.6% reduction in BSI rates so far in 2018. We are on track to meet our target of a 50% reduction.
Implications:
The RCA findings have shown that there are a number of factors which contribute to a patient developing BSI. This means a number of different strategies are needed to improve BSI rates.
Future work includes
• develop an e-learning module for PN
• trial some ward-based Care of CVC update training for nurses
This improvement programme has focused on BSI in patients receiving PN but it could also be applied to improving the care of all CVCs in all our patients.
References (1) Pironi L, Arends J, Bozzetti F, et al ESPEN Guidelines on chronic intestinal failure in adults. Clinical Nutrition. 2016; 35 (2) 247-307.
(2) NICE - Curos disinfecting cap for needleless connectors. Available from: https://www.nice.org.uk/advice... [Accessed 24th August 2018].