Some AEC models tackle this by adopting a case finding approach, this may involve screening referrals from primary care or regular visits to the ED to identify patients with suspected DVT or cellulitis that would fit the pathway. This increases the number of patients but is still constrained by only having a limited number of pathways. The next step often involves increasing the number of pathways available to between 5-10. Typically this would include, suspected PE, low risk chest pain, first fits, transient loss of consciousness etc. Expanding the number of pathways will increase AEC activity, however, the pathways still act as a constraint. At this point, the pressure is to write more pathways, potentially rewriting a text book as there are 49 clinical scenarios in the directory and we are aware of other presentations managed through AEC which are not yet in the directory. There is also a point of diminishing returns here as the number of patients on each successive pathway will decline, a lot of effort for little return.
Of course real life medicine is not like this. In the emergency setting we do not know what the next clinical presentation will be, however, we are prepared to receive the patient and provide the best possible care. How would such an approach operate in the AEC setting? We call this the process approach.
What is the process approach? Essentially it involves 4 steps
- Identifying the clinical severity of the patient - this is done by a clinical conversation support by clinical observations
- Establishing whether the patient’s clinical needs can be best met by the AEC service
- Ensuring the staffing and environment are appropriate to maintain the patients privacy & dignity
- Confirming that this is an emergency presentation and not an urgent out-patient clinic
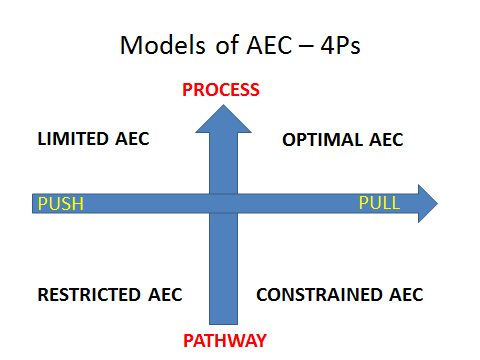
The response to this evaluation will determine whether or not the patient can be effectively managed in the AEC service. However, it still needs a case finding approach to optimise the service. This appears to be best done by consultant telephone streaming of GP referrals and attendance at ED board rounds. In practice then the patient identification requires process and pull supported by pathways for the most common clinical presentations to standardise care, drive out variation and maintain safety. This will ensure that we identify the right patients to be treated in the right place at the right time.
Dr Vincent Connolly -Consultant Physician, The James Cook University Hospital Middlesbrough & Medical Director, Emergency Care Improvement Programme (ECIP) @vincentconnolly
