
North Tees and Hartlepool NHS Foundation Trust is focussed on “excellence as our standard” and we are on a continuous learning and transformation journey to improve services for our patients.
In January 2020, Quality Improvement (QI) Clinical Fellows were recruited as part of Chief Pharmacist’s office. We would like to share an example of such QI achievement by Kevin Irvine appointed as one of the QI Clinical Pharmacists, specialising in Cardiovascular and Anticoagulation Medicine.
Dr Mojgan H Sani, Director Medicines Optimisation & Chief Pharmacist said “we are so pleased to be able demonstrate the value of these QI initiatives for improving patient care and use of medicines in an appropriate and safe manner”.
Here is Kevin’s summary of his QI initiative.
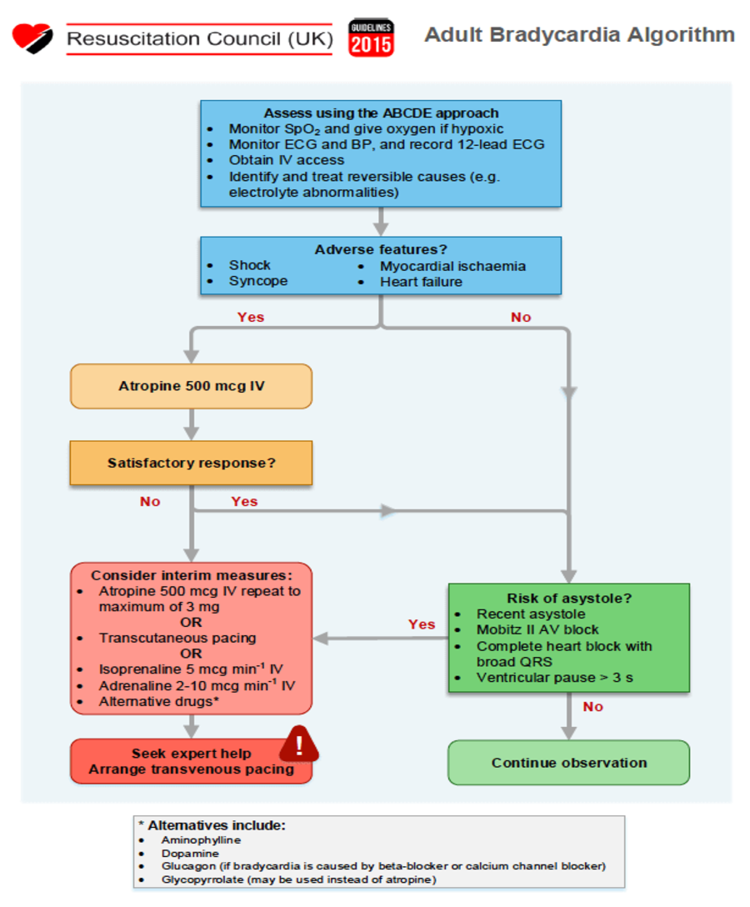
Isoprenaline is a sympathomimetic that acts almost exclusively on beta-adrenergic receptors. It has a powerful stimulating action on the heart and increases cardiac output, excitability, and rate. It has been ratified by the Resuscitation UK guidelines 2015 as a suitable treatment option for patients who present to hospital with severe bradycardia and who are unresponsive to atropine. It can be used instead of transcutaneous pacing which can be very invasive for patients and needs to be carried out by cardiac specialists. The Resuscitation Council UK algorithm for bradycardia can be seen below:1
Why did we need a protocol?
Severe bradycardia can trigger CARDIAC ARREST:
The instance of in-hospital cardiac arrest is 1.6 per 1000 hospital admissions in the UK. Currently there are approx. 15.8m hospital admissions per year and this puts the total number of in-hospital cardiac arrests at over 25,000.2 Of these 25,000 patients over 80% will not recover to discharge and this results in more than 20,000 in-hospital deaths per year.2 Studies have shown that of these 20,000 deaths, more than 38% are preventable and this figure represents 7700 avoidable deaths.2 This would equate to more than 50 avoidable deaths each year for each UK NHS trust.2
Patients who present to the front of house areas such as A&E, Urgent care, and EAU may not be able to receive treatment with Isoprenaline in a timely manner due to a number of factors including clinical staff not being familiar with the medication, medication not stocked in the correct area, and most importantly staff not having a protocol to follow. As the general population gets older we are likely to see more patients attending hospital with bradycardia. It has been deemed a vital medication by the cardiology team and that front of house clinical staff should become more familiar with its use to improve patient safety and reduce the need for pacing and even hospital admissions.
How was the protocol developed?
I recently joined the trust in the middle of the national pandemic in April 2020. My chosen clinical specialty is cardiology and I was approached by the team to develop this protocol as a quality improvement initiative. I liaised with the cardiology team who were very keen for the development of a trust protocol that could be used by all staff members and not just cardiology specialty. Isoprenaline is a high risk antiarrhythmic medication that can be potentially lifesaving but can also cause serious adverse effects and therefore a protocol needed to be developed to ensure patient safety.
A draft protocol was initially put together and shared with the cardiology team and various other consultants including acute medicine, critical care, emergency department and others. Feedback on the draft protocol was received which included confusion between various forms of Isoprenaline stocked within the hospital. It was discovered that both Isoprenaline hydrochloride and sulphate were kept in different areas. I worked with the Omnicell pharmacy technician within the department to ensure that the sulphate formulation was removed from all omnicells within the trust. I amended the rates of administration and made the method of administration clearer for clinical staff. Finally, I sent the protocol for further discussion with the relevant clinicians for more feedback before sending the protocol to the Clinical Guidelines Committee for final approval. The protocol has now been shared on the trust intranet and can be accessed by all members of staff. The implementation of this guideline will mean that more patients can be treated acutely in the future which will ultimately lead to fewer hospital admissions and improve patient outcomes going forward. Finally, the protocol has been welcomed by all consultants and been ratified by the cardiology team.
What information does the protocol include?
The protocol is split into a few main sections including:
- Aim
- Cautions
- Adverse effects
- Monitoring requirements
- Locations where the medication is stocked
- Method of administration (including emergency administration)
- Rate of administration tables
- References
How do we measure its effectiveness?
By liaising with our Medications Safety Officer (MSO) we can check if the number of Datix incident reports relating to Isoprenaline are reduced over the next few months. I will also acquire feedback from the clinical areas using the protocol to administer Isoprenaline.
Conclusion:
Going forward, there is a significant body of evidence from literature that clinical pharmacists are best placed, as experts in medicines following 8 years of Masters and postgraduate education, to lead on development and implementation of clinical medicines guidelines, and monitor effectiveness within the multidisciplinary teams. Clinical pharmacists have been an underutilised profession in the past but I believe that this is changing throughout the NHS and has led to better care for our patients. I aim to be involved in much more quality improvement work in the future.
References:
1:Resuscitation Council UK Guidelines: Treatment of Symptomatic Bradycardia. Adult
Bradycardia Algorithm G2015 (Accessed August 2020)
2. Ltd S. Patient deterioration [Internet]. Patient deterioration. 2020 [cited 21 August 2020]. Available from: https://www.sensium.co.uk/patient-deterioration/
Author:
Kevin Irvine (QI Clinical Pharmacist Fellow & Cardiovascular Specialist)
Acknowledgement:
I would like to thank the cardiology team at North Tees and Hartlepool Foundation Trust for their support in the development of this guideline. In particular, Dr. Matthew Dewhurst for overseeing the process.


