Oncology patients are often referred to a nuclear medicine department to undergo a radioisotope bone scan.
This is a functional imaging test to look for metastatic cancer which can often metastasise to the bones.
The patient is given an injection of a radiopharmaceutical and is scanned two hours later using a gamma camera.
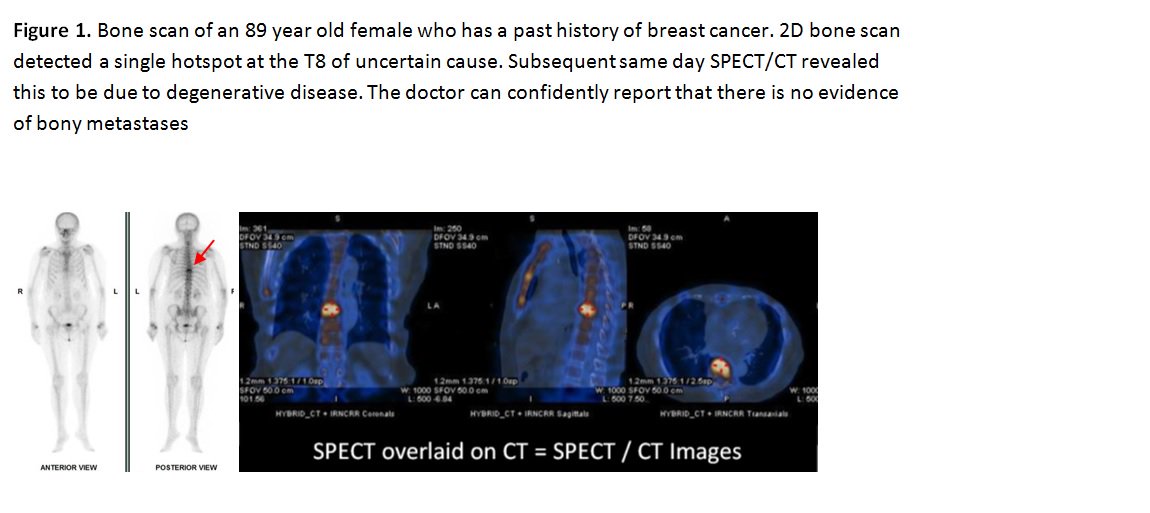
The standard 2D bone scan is quite sensitive to any abnormality that could potentially be caused by cancer. These are represented by high uptake of injected radiopharmaceutical, often referred to as a ‘hotspot’.
 But for approximately 50% of patients, the final results can sometimes be indeterminate. This is because patients often have non-metastatic hotspots caused by degenerative conditions or old fractures. Such uncertainty results in the patient being referred to the x-ray department for an additional CT scan to obtain structural images to help clarify the cause of the hotspot.
But for approximately 50% of patients, the final results can sometimes be indeterminate. This is because patients often have non-metastatic hotspots caused by degenerative conditions or old fractures. Such uncertainty results in the patient being referred to the x-ray department for an additional CT scan to obtain structural images to help clarify the cause of the hotspot.This leads to delays in diagnosis, delays in getting onto the right course of treatment, and anxiety whilst waiting for an appointment. The health service has to pay for costs associated with referral, performing and reporting of the scan. Reporting the bone scan and CT scan side-by-side are not always straightforward as the location of the hot spot may not be obvious on the CT.
This problem has been solved since the introduction of a SPECT-CT scanner. This is used to examine in more detail any areas of concern found on the bone scan by producing functional and structural 3D images of the bones simultaneously.
These pictures are fused together to produce hybrid images, whereby the location of any hotspot can be immediately found on the CT scan. For the radiologist, these hybrid pictures are easier to report and have better sensitivity, better specificity and produce more certain ‘clear-cut’ results.
The patient receives better care by getting their diagnosis sooner thus being put on the right treatment plan in a shorter time. The introduction of SPECT-CT for oncology bone imaging raised several significant challenges.
The need for SPECT-CT is not known until the bone scan pictures are taken. The decision rests with the radiologist who is not always available. Additional scans take extra time which could impact on the capacity of the department.
A team meeting was held and we set out to create a service whereby the correct decision to proceed to a SPECT/CT is made without the need to wait for a medic to immediately review the images.
Instead, this is made by the clinical scientists and practitioners after they had been trained by participation in reporting sessions. This is cost effective, and streamlined for the patient’s convenience, improves accuracy of the diagnostic test, and at the same time avoids unnecessary imaging with associated cost and radiation to the patient.
 A workplan was introduced to better schedule bone scans, minimising patients waiting for SPECT-CT on the day.
A workplan was introduced to better schedule bone scans, minimising patients waiting for SPECT-CT on the day.The current practice is now well established and we have presented our protocol and workplan at the national British Nuclear Medicine Society (BNMS) meeting.