Background: remote behavioural support impedes carbon monoxide (CO) monitoring to validate a quit. And self-reporting of being and remaining smokefree is not accurate and creates errors with validating smoking-at-time-of-delivery (SATOD) data. In April 2021, the Mums2Be Smokefree Service started a 12-month Bluetooth CO (iCOquit) monitor pilot to support service users remotely to quit smoking and remain quit throughout their pregnancy and post-partum. The pilot enabled comparison of routine quit and loss-to-follow-up (LTFU) data pre- and post-pilot, and evaluation of the value of the iCOquit monitor as experienced by service users and Stop Smoking Practitioners. Accordingly, evaluation research was embedded in the pilot.
Aims of the evaluation research: to evaluate if the iCOquit monitor enables service users to strengthen self-care skills to quit smoking and remain quit. And to evaluate if the monitor enables Stop Smoking Practitioners to strengthen sustained support for service users.
Design of the mixed-method evaluation: a structured outcome evaluation was conducted using a mini digital survey with a nested qualitative component consisting of semi-structured and unstructured questions. A brief semi-structured questionnaire was used to evaluate the iCOquit monitor integration experiences of the Stop Smoking Practitioners. Ethics approval for the research was obtained from Somerset County Council.
Study population and sample: purposive sampling included all adult service users (N=58) in the pilot who received an iCOquit monitor from the Service at 4-weeks (n=20, 34%) or 12-weeks (n=38, 66%) pregnant since 1 April 2022, and who had not quit or were LTFU. Out of the total population (N=58), 51 (88%) confirmed their participation, and 29 (50%) completed the questionnaire. All Mums2Be Smokefree Practitioners (N=5, 100%) completed a brief evaluation questionnaire.
Data analysis: the pilot sample quit outcomes were analysed, followed by comparison of the routine quit rates and LTFU service data during quarters-1 and 4 in 2020/21 (pre-pilot) and 2021/22 (post-pilot). Simple descriptive analysis of the quantitative, and thematic analysis of the qualitative, survey data were undertaken.
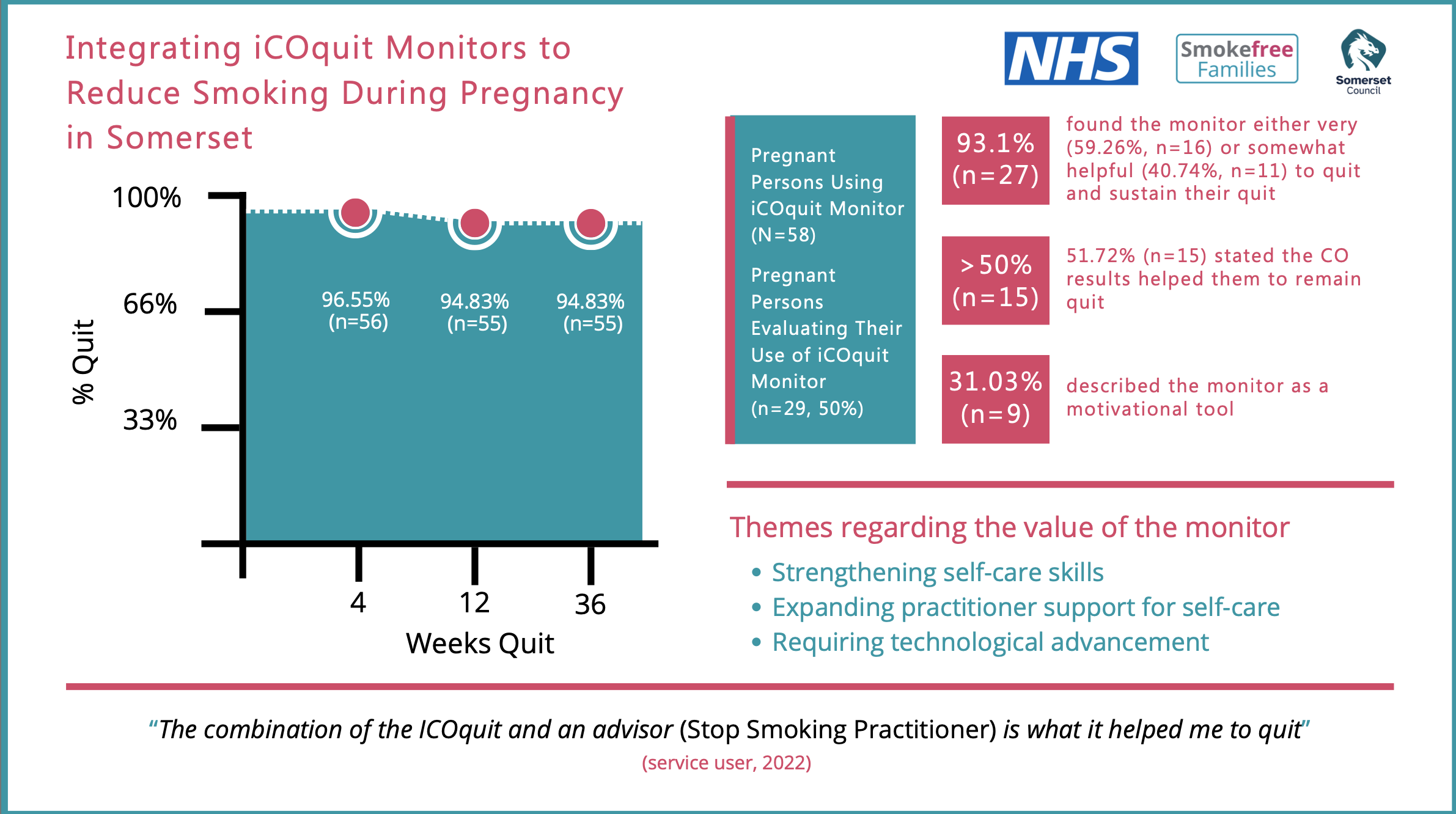
Findings: quit rates increased at 4-weeks (96.55%, n=56), 12-weeks (94.83%, n=55) and 36-weeks (94.83%, n=55), significantly above the service standard; 4- and 12-weeks CO validations increased by 100%, marked by 62.8% (n=130) of 4-weeks quits, and 67.88% (n=112) of 12-weeks quits; LTFU and not quits at 4-weeks decreased by 3.94% (n=7) and 9.36% (n=24) respectively; and LTFU and not quits at 12-weeks decreased by 4.16% (n=1) and 2-weeks by 1.87% (n=5). Most participants (93.1%, n=27) found the monitor either very (59.26%, n=16) or somewhat helpful (40.74%, n=11) to quit and sustain their quit. Over half (51.72%, n=15) stated that seeing the iCOquit monitor results supported them to remain quit. Two qualitative themes confirm the value of the iCOquit monitor by Strengthening Self-Care Skills, and by Expanding Practitioner Support. Another theme highlights the Need for Technological Advancement of the monitor:
Conclusion: the findings suggest that the iCOquit monitor improved quit outcomes in pregnancy by supporting self-care skills and by enabling Stop Smoking Practitioners to strengthen sustained support for service users. Furthermore, the findings underscore the importance of behavioural support in addition to integration of the iCOquit monitor. Despite certain limitations, such as the small evaluation sample size and not being able to establish the reasons for the total population not completing the anonymous online survey, the findings from the evaluation research yielded several learnings coupled with participant and practitioner recommendations for strengthening the integration of the iCOquit monitor. These findings could be of value to policies and practices in other settings towards enabling services users and Stop Smoking Practitioners
You can read and download the full report HERE